Pulmonary Hypertension Research Paper
Pulmonary hypertension is a type of high blood pressure that affects the arteries in your lungs and the right side of your heart.
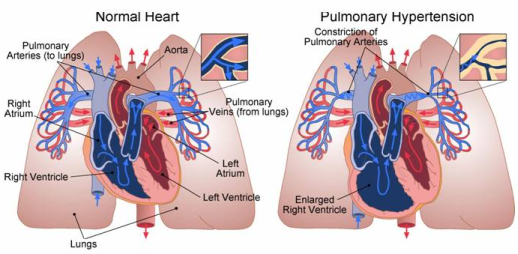
In one form of pulmonary hypertension, tiny arteries in your lungs, called pulmonary arterioles, and capillaries become narrowed, blocked or destroyed. This makes it harder for blood to flow through your lungs, and raises pressure within your lung's arteries. As the pressure builds, your heart's lower right chamber (right ventricle) must work harder to pump blood through your lungs, eventually causing your heart muscle to weaken and fail.Pulmonary Hypertension Research Paper
ORDER A PLAGIARISM-FREE PAPER HERE
Some forms of pulmonary hypertension are serious conditions that become progressively worse and are sometimes fatal. Although some forms of pulmonary hypertension aren't curable, treatment can help lessen symptoms and improve your quality of life.
Symptoms
The signs and symptoms of pulmonary hypertension in its early stages might not be noticeable for months or even years. As the disease progresses, symptoms become worse.
Pulmonary hypertension symptoms include:
- Shortness of breath (dyspnea), initially while exercising and eventually while at rest
- Fatigue
- Dizziness or fainting spells (syncope)
- Chest pressure or pain
- Swelling (edema) in your ankles, legs and eventually in your abdomen (ascites)
- Bluish color to your lips and skin (cyanosis)
- Racing pulse or heart palpitations
Causes
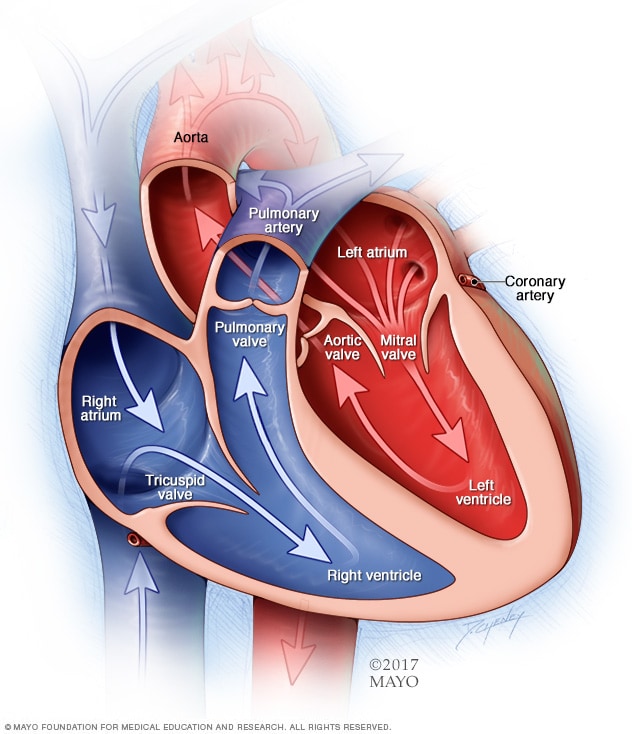
Your heart has two upper chambers (atria) and two lower chambers (ventricles). Each time blood passes through your heart, the lower right chamber (right ventricle) pumps blood to your lungs through a large blood vessel (pulmonary artery).Pulmonary Hypertension Research Paper
-
Chambers and valves of the heartn your lungs, the blood releases carbon dioxide and picks up oxygen. The oxygen-rich blood then flows through blood vessels in your lungs (pulmonary arteries, capillaries and veins) to the left side of your heart. Ordinarily, the blood flows easily through the vessels in your lungs, so blood pressure is usually much lower in your lungs.
With pulmonary hypertension, the rise in blood pressure is caused by changes in the cells that line your pulmonary arteries. These changes can cause the walls of the arteries to become stiff and thick, and extra tissue may form. The blood vessels may also become inflamed and tight.
These changes in the pulmonary arteries can reduce or block blood flow through the blood vessels. This makes it harder for blood to flow, raising the blood pressure in the pulmonary arteries.Pulmonary Hypertension Research Paper
-
Pulmonary hypertension
Pulmonary hypertension is classified into five groups, depending on the cause.
Group 1: Pulmonary arterial hypertension
- Cause unknown, known as idiopathic pulmonary arterial hypertension
- A specific gene mutation that can cause pulmonary hypertension to develop in families, also called heritable pulmonary arterial hypertension
- Certain drugs — such as certain prescription diet drugs or illegal drugs such as methamphetamines — or certain toxins
- Heart abnormalities present at birth (congenital heart disease)
- Other conditions, such as connective tissue disorders (scleroderma, lupus, others), HIV infection or chronic liver disease (cirrhosis)
Group 2: Pulmonary hypertension caused by left-sided heart disease
- Left-sided valvular heart disease, such as mitral valve or aortic valve disease
- Failure of the lower left heart chamber (left ventricle)
Group 3: Pulmonary hypertension caused by lung disease
- Chronic obstructive pulmonary disease, such as emphysema
- Lung disease such as pulmonary fibrosis, a condition that causes scarring in the tissue between the lungs' air sacs (interstitium)
- Sleep apnea and other sleep disorders
- Long-term exposure to high altitudes in people who may be at higher risk of pulmonary hypertension
Group 4: Pulmonary hypertension caused by chronic blood clots
- Chronic blood clots in the lungs (pulmonary emboli)
Group 5: Pulmonary hypertension associated with other conditions that have unclear reasons why the pulmonary hypertension occurs
- Blood disorders
- Disorders that affect several organs in the body, such as sarcoidosis
- Metabolic disorders, such as glycogen storage disease
- Tumors pressing against pulmonary arteries
Eisenmenger syndrome and pulmonary hypertension
Eisenmenger syndrome, a type of congenital heart disease, causes pulmonary hypertension. It's most commonly caused by a large hole in your heart between the two lower heart chambers (ventricles), called a ventricular septal defect.Pulmonary Hypertension Research Paper
This hole in your heart causes blood to circulate abnormally in your heart. Oxygen-carrying blood (red blood) mixes with oxygen-poor blood (blue blood). The blood then returns to your lungs instead of going to the rest of your body, increasing the pressure in the pulmonary arteries and causing pulmonary hypertension.
Risk factors
Your risk of developing pulmonary hypertension may be greater if:
- You're a young adult, as idiopathic pulmonary arterial hypertension is more common in younger adults
- You're overweight
- You have a family history of the disease
- You have one of various conditions that can increase your risk of developing pulmonary hypertension
- You use illegal drugs, such as cocaine
- You take certain appetite-suppressant medications
- You have an existing risk of developing pulmonary hypertension, such as a family history of the condition, and you live at a high altitude
Complications
Pulmonary hypertension can lead to a number of complications, including:
- Right-sided heart enlargement and heart failure (cor pulmonale). In cor pulmonale, your heart's right ventricle becomes enlarged and has to pump harder than usual to move blood through narrowed or blocked pulmonary arteries.At first, the heart tries to compensate by thickening its walls and expanding the chamber of the right ventricle to increase the amount of blood it can hold. But this thickening and enlarging works only temporarily, and eventually the right ventricle fails from the extra strain.
- Blood clots. Clots help stop bleeding after you've been injured. But sometimes clots form where they're not needed. A number of small clots or just a few large ones dislodge from these veins and travel to the lungs, leading to a form of pulmonary hypertension that can generally be reversible with time and treatment.Having pulmonary hypertension makes it more likely you'll develop clots in the small arteries in your lungs, which is dangerous if you already have narrowed or blocked blood vessels.Pulmonary Hypertension Research Paper
- Arrhythmia. Irregular heartbeats (arrhythmias) from the upper or lower chambers of the heart are complications of pulmonary hypertension. These can lead to palpitations, dizziness or fainting and can be fatal.
- Bleeding. Pulmonary hypertension can lead to bleeding into the lungs and coughing up blood (hemoptysis). This is another potentially fatal complication.
What is pulmonary hypertension?
Pulmonary hypertension (PHT) is high blood pressure in the heart-to-lung system that delivers fresh (oxygenated) blood to the heart while returning used (oxygen-depleted) blood back to the lungs.
Pulmonary versus systemic blood pressure
Unlike systemic blood pressure, which represents the force of your blood moving through the blood vessels in your body, pulmonary blood pressure reflects the pressure the heart exerts to pump blood from the heart through the arteries of the lungs. In other words, it focuses on the pressure of the blood flow in your lungs.
How blood flows through your heart and lungs
The lower right heart chamber, the right ventricle, receives oxygen-depleted blood and pumps it to your pulmonary arteries. The blood then travels to your lungs to be oxygenated, and on to the upper left heart chamber, the left atrium. From there, the oxygen-rich blood moves into the lower left chamber, the left ventricle, which pumps blood to the rest of your body through the aorta.Pulmonary Hypertension Research Paper
The numbers in pulmonary hypertension
Pulmonary blood pressure is normally a lot lower than systemic blood pressure. Normal pulmonary artery pressure is 8-20 mm Hg at rest. If the pressure in the pulmonary artery is greater than 25 mm Hg at rest or 30 mmHg during physical activity, it is abnormally high and is called pulmonary hypertension.
The long-term effects of pulmonary hypertension
Similar to how systemic high blood pressure can cause the heart to work harder to deliver blood to the body, pulmonary hypertension can occur when the arteries in the lungs narrow and thicken, slowing the flow of blood through the pulmonary arteries to the lungs. As a result, the pressure in your arteries rises as your heart works harder to try to force the blood through. Heart failure occurs when the heart becomes too weak to pump enough blood to the lungs.
ORDER A PLAGIARISM-FREE PAPER HERE
Symptoms of pulmonary hypertension
Early symptoms include:
- Shortness of breath during routine activity
- Fatigue
- Chest pain
- Racing heartbeat
- Pain in upper right side of abdomen
- Decreased appetite
Later symptoms include:
- Feeling light-headed, especially during physical activity
- Fainting
- Swelling in the ankles or legs
- Bluish lips or skin
Diagnosis and treatment
Pulmonary hypertension can develop slowly, without early signs and symptoms. When symptoms do occur, they may be attributed to asthma or other lung or heart conditions.Pulmonary Hypertension Research Paper
To diagnose pulmonary hypertension, your doctor may ask about your symptoms and risk factors, including other medical conditions and family history. Having a family member with pulmonary hypertension increases your risk of developing the disease.
Medical evaluation
Your physician may recommend tests and procedures to diagnose pulmonary hypertension and discover its cause and severity. Common diagnostic tests include an echo cardiograph, chest X-ray, electrocardiogram (EKG) and catheterization of the right heart. Discovering the underlying cause may involve a chest CT scan, chest MRI, lung function tests, polysomnogram (PSG), lung ventilation/perfusion scan and blood tests.Pulmonary Hypertension Research Paper
Once you have a diagnosis of pulmonary hypertension, exercise testing can help your doctor determine its severity. The test measures how well your heart and lungs work while you are on a treadmill or bicycle, so the doctor can rate your activity level. Exercise testing may be ongoing during your treatment in order to monitor your progress.
Types of pulmonary hypertension
The World Health Organization has established five groups of pulmonary hypertension.
Group 1 pulmonary arterial hypertension (PAH)
Group 1 PAH includes pulmonary hypertension that has no known cause; is inherited; is caused by drugs or toxins; is caused by conditions such as connective tissue disease, HIV infection, liver disease, congenital heart disease, sickle cell disease, or schistosomiasis; or is caused by conditions that affect the veins and small blood vessels of the lungs.
Group 2 pulmonary hypertension
Group 2 pulmonary hypertension is often associated with left heart disease such as mitral valve disease or long-term high blood pressure. Left heart disease is the most common cause of pulmonary hypertension.Pulmonary Hypertension Research Paper
Group 3 pulmonary hypertension
Group 3 is related to lung problems like chronic obstructive pulmonary disease (COPD) and interstitial lung disease, as well as sleep apnea and other sleep-related breathing disorders.
Group 4 pulmonary hypertension
Group 4 includes pulmonary hypertension caused by blood clots in the lungs or general clotting disorders.
Group 5 pulmonary hypertension
Group 5 includes pulmonary hypertension triggered by other disorders. Examples of such diseases or conditions are blood disorders such as polycythemia vera and essential thrombocythemia; systemic disorders such as sarcoidosis and vasculitis; metabolic disorders such as thyroid and glycogen storage disease; and other conditions such as kidney disease and tumors that press on the pulmonary arteries.
Factors that can affect pulmonary hypertension
While pulmonary hypertension has no cure, you can live an active, fulfilling life by working with your doctor to manage your symptoms. Talk to your doctor before taking over-the-counter medicine, as some can worsen symptoms of pulmonary hypertension or interfere with prescriptions — and keep a list of medicines with you. Ask whether you should get a pneumonia vaccination or flu shot. Additionally, pregnancy can pose serious risks for women with pulmonary hypertension, so be sure to discuss birth control options with your physician.Pulmonary Hypertension Research Paper
These lifestyle changes can improve your symptoms:
- Quit smoking. Your doctor can recommend programs and products to help.
- Follow a healthy diet. Eat a variety of fruits, vegetables, and whole grains, plus lean meat, poultry, fish and low-fat/fat-free milk. Your diet should be low in fat, cholesterol, sodium and sugar.
- Watch your weight. A daily record of your weight can help you be aware of rapid weight gain, which may be a sign that your pulmonary hypertension is worsening.
- Stay active. Incorporate physical activity such as walking into your lifestyle. Discuss the level of activity with your doctor. Avoid straining or lifting heavy weights. Rest when you need to.
- Avoid sitting in a hot tub or sauna, or taking long baths, which will lower your blood pressure.
- Be cautious about air travel or high-altitude locales. You may need to travel with extra oxygen.
- Get support for the anxiety and stress of living with pulmonary hypertension. Talk with your healthcare team, or ask for a referral to a counselor. A support group for people living with pulmonary hypertension can be invaluable in learning how to cope with the illness.
Pulmonary hypertension is hard to diagnose early because it's not often detected in a routine physical exam. Even when the condition is more advanced, its signs and symptoms are similar to those of other heart and lung conditions.Pulmonary Hypertension Research Paper
To diagnose your condition, your doctor may review your medical and family history, discuss your signs and symptoms, and conduct a physical examination. Doctors may order several tests to diagnose pulmonary hypertension, determine the severity of your condition and find out the cause of your condition. Tests may include:
- Echo cardiogram. Sound waves can create moving images of the beating heart. An echo cardiogram can help your doctor to check the size and functioning of the right ventricle, and the thickness of the right ventricle's wall. An echo cardiogram can also show how well your heart chambers and valves are working. Doctors may also use this to measure the pressure in your pulmonary arteries.In some cases, your doctor will recommend an exercise echo cardiogram to help determine how well your heart and lungs work under stress. In this test, you'll have an echo cardiogram before exercising on a stationary bike or treadmill and another test immediately afterward. This could be done as an oxygen consumption test, in which you may have to wear a mask that assesses the ability of your heart and lungs to deal with oxygen and carbon dioxide.Pulmonary Hypertension Research Paper
Other exercise tests may also be done. These tests can help determine the severity and cause of your condition. They may also be done at follow-up appointments to check that your treatments are working.
- Chest X-ray. A chest X-ray can show images of your heart, lungs and chest. This test can show enlargement of the right ventricle of the heart or the pulmonary arteries, which can occur in pulmonary hypertension. This test can also be used to identify other conditions that may be causing pulmonary hypertension.
- Electrocardiogram (ECG). This noninvasive test shows your heart's electrical patterns and can detect abnormal rhythms. Doctors may also be able to see signs of right ventricle enlargement or strain.
- Right heart catheterization. After you've had an echo cardiogram, if your doctor thinks you have pulmonary hypertension, you'll likely have a right heart catheterization. This test can often help confirm that you have pulmonary hypertension and determine the severity of your condition.During the procedure, a cardiologist places a thin, flexible tube (catheter) into a vein in your neck or groin. The catheter is then threaded into your right ventricle and pulmonary artery.
Right heart catheterization allows your doctor to directly measure the pressure in the main pulmonary arteries and right ventricle. It's also used to see what effect different medications may have on your pulmonary hypertension.
- Blood tests. Your doctor might order blood tests to check for certain substances in your blood that might show you have pulmonary hypertension or its complications. Blood tests can also test for certain conditions that may be causing your condition.Pulmonary Hypertension Research Paper
Your doctor might order additional tests to check the condition of your lungs and pulmonary arteries and to determine the cause of your condition, including:
- Computerized tomography (CT) scan. During a CT scan, you lie on a table inside a doughnut-shaped machine. CT scanning generates X-rays to produce cross-sectional images of your body. Doctors may inject a dye into your blood vessels that helps your arteries to be more visible on the CT pictures (CT angiography).Doctors may use this test to look at the heart's size and function and to check for blood clots in the lungs' arteries.
- Magnetic resonance imaging (MRI). This test may be used to check the right ventricle's function and the blood flow in the lung's arteries. In this test, you lie on a movable table that slides into the tunnel. An MRI uses a magnetic field and pulses of radio wave energy to make pictures of the body.
- Pulmonary function test. This noninvasive test measures how much air your lungs can hold, and the airflow in and out of your lungs. During the test, you'll blow into a simple instrument called a spirometer.
- Polysomnogram. This test detects your brain activity, heart rate, blood pressure, oxygen levels and other factors while you sleep. It can help diagnose a sleep disorder such as obstructive sleep apnea.
- Ventilation/perfusion (V/Q) scan. In this test, a tracer is injected into a vein in your arm. The tracer maps blood flow and air to your lungs. This test can be used to determine whether blood clots are causing symptoms of pulmonary hypertension.Pulmonary Hypertension Research Paper
- Open-lung biopsy. Rarely, a doctor might recommend an open-lung biopsy. An open-lung biopsy is a type of surgery in which a small sample of tissue is removed from your lungs under general anesthesia to check for a possible secondary cause of pulmonary hypertension.
Genetic tests
If a family member has had pulmonary hypertension, your doctor might screen you for genes that are linked with pulmonary hypertension. If you test positive, your doctor might recommend that other family members be screened for the same genetic mutation.
Pulmonary hypertension classifications
Once you've been diagnosed with pulmonary hypertension, your doctor might classify the severity of your disease into one of several classes, including:
- Class I. Although you've been diagnosed with pulmonary hypertension, you have no symptoms with normal activity.
- Class II. You don't have symptoms at rest, but you experience symptoms such as fatigue, shortness of breath or chest pain with normal activity.
- Class III. You're comfortable at rest, but have symptoms when you're physically active.
- Class IV. You have symptoms with physical activity and while at rest.Pulmonary Hypertension Research Paper
Treatment
Pulmonary hypertension can't be cured, but doctors can help you manage your condition. Treatment may help improve your symptoms and slow the progress of pulmonary hypertension.
It often takes some time to find the most appropriate treatment for pulmonary hypertension. The treatments are often complex and require extensive follow-up care. Your doctor might also need to change your treatment if it's no longer effective.
When pulmonary hypertension is caused by another condition, your doctor will treat the underlying cause whenever possible.
Medications
- Blood vessel dilators (vasodilators). Vasodilators open narrowed blood vessels. One of the most commonly prescribed vasodilators for pulmonary hypertension is epoprostenol (Flolan, Veletri). The drawback to epoprostenol is that its effects last only a few minutes.This drug is continuously injected through an intravenous (IV) catheter via a small pump that you wear in a pack on your belt or shoulder. Potential side effects of epoprostenol include jaw pain, nausea, diarrhea and leg cramps, as well as pain and infection at the IV site.
Another form of the drug, iloprost (Ventavis), can be inhaled six to nine times a day through a nebulizer, a machine that vaporizes your medication. Because it's inhaled, it goes directly to the lungs. Side effects associated with iloprost include chest pain — often accompanied by a headache and nausea — and breathlessness.
Treprostinil (Tyvaso, Remodulin, Orenitram), another form of the drug, can be given four times a day. It can be inhaled, taken as oral medication or administered by injection. It can cause side effects such as a headache, nausea and diarrhea.
- Endothelin receptor antagonists. These medications reverse the effect of endothelin, a substance in the walls of blood vessels that causes them to narrow. These drugs may improve your energy level and symptoms. However, these drugs shouldn't be taken if you're pregnant. Also, these drugs can damage your liver and you may need monthly liver monitoring.These medications include bosentan (Tracleer), macitentan (Opsumit), and ambrisentan (Letairis).
- Sildenafil and tadalafil. Sildenafil (Revatio, Viagra) and tadalafil (Cialis, Adcirca) are sometimes used to treat pulmonary hypertension. These drugs work by opening the blood vessels in the lungs to allow blood to flow through more easily. Side effects can include an upset stomach, headache and vision problems.Pulmonary Hypertension Research Paper
- High-dose calcium channel blockers. These drugs help relax the muscles in the walls of your blood vessels. They include medications such as amlodipine (Norvasc), diltiazem (Cardizem, Tiazac, others) and nifedipine (Procardia, others). Although calcium channel blockers can be effective, only a small number of people with pulmonary hypertension respond to them.
- Soluble guanylate cyclase (SGC) stimulator. Soluble guanylate cyclase (SGC) stimulators (Adempas) interact with nitric oxide and help relax the pulmonary arteries and lower the pressure within the arteries. These medications should not be taken if you're pregnant. They can sometimes cause dizziness or nausea.
- Anticoagulants. Your doctor is likely to prescribe the anticoagulant warfarin (Coumadin, Jantoven) to help prevent the formation of blood clots within the small pulmonary arteries. Because anticoagulants prevent normal blood coagulation, they increase your risk of bleeding complications.Take warfarin exactly as prescribed, because warfarin can cause severe side effects if taken incorrectly. If you're taking warfarin, your doctor will ask you to have periodic blood tests to check how well the drug is working. Many other drugs, herbal supplements and foods can interact with warfarin, so be sure your doctor knows all of the medications you're taking.
- Digoxin. Digoxin (Lanoxin) can help the heart beat stronger and pump more blood. It can help control the heart rate if you experience arrhythmias.
- Diuretics. Commonly known as water pills, these medications help eliminate excess fluid from your body. This reduces the amount of work your heart has to do. They may also be used to limit fluid buildup in your lungs.
- Oxygen. Your doctor might suggest that you sometimes breathe pure oxygen, a treatment known as oxygen therapy, to help treat pulmonary hypertension, especially if you live at a high altitude or have sleep apnea. Some people who have pulmonary hypertension eventually require continuous oxygen therapy.Pulmonary Hypertension Research Paper
Surgeries
- Atrial septostomy. If medications don't control your pulmonary hypertension, this open-heart surgery might be an option. In an atrial septostomy, a surgeon will create an opening between the upper left and right chambers of your heart (atria) to relieve the pressure on the right side of your heart.Atrial septostomy can have serious complications, including heart rhythm abnormalities (arrhythmias).
- Transplantation. In some cases, a lung or heart-lung transplant might be an option, especially for younger people who have idiopathic pulmonary arterial hypertension.Major risks of any type of transplantation include rejection of the transplanted organ and serious infection, and you must take immunosuppressant drugs for life to help reduce the chance of rejection.
Pulmonary hypertension (PH) is a rare, life-threatening disease characterized by high blood pressure in the lungs due to damage to the pulmonary arteries. These vessels, which are responsible for transporting blood from the heart to the lungs, become narrowed and blocked due to the disease. Therefore, the heart needs to work harder to properly pump the blood, becoming enlarged and weakened. Patients are particularly at risk of developing other conditions and suffering right heart failure.Pulmonary Hypertension Research Paper
There is currently no cure for pulmonary hypertension, but there are treatments that can help ease the symptoms, slow the progression of the disease and improve patients’ quality of life. According to the National Heart, Lung and Blood Institute (NHLB) from the National Institutes of Health (NIH), PH is treated with medicines, procedures, and other therapies, which are prescribed based on the subtype of the disease diagnosed as well as its severity.
How to Treat Pulmonary Arterial Hypertension: Group 1
The group 1 defined by the World Health Organization (WHO) includes inherited or familial PH and idiopathic PH, which means that the cause for it is unknown, as well as PH caused by determined drugs or conditions. Medication is one of the courses of treatment for group 1 pulmonary arterial hypertension. The most common drugs are meant to relax the blood vessels in the lungs and reduce excess cell growth in the blood vessels. Medication, which can be taken orally, inhaled or injected, include phosphodiesterase-5 inhibitors such as sildenafil, prostanoids, such as epoprostenol, endothelin receptor antagonists, such as bosentan and ambrisentan, and calcium channel blockers, such as diltiazem.
Physicians can prescribe one or more medications, as well as request an acute vasoreactivity test to evaluate how the pressure in the pulmonary arteries reacts to prescribed drugs. In addition, the doctor may also recommend medical and surgical procedures. During an atrial septostomy (sep-TOS-toe-me), a catheter is placed through a blood vessel of the leg into the heart’s septum, which is the wall that separates the left and right atria. A tiny balloon on the tip of the tube is then inflated, creating an opening between the atria and relieving the pressure. While the atrial septostomy is a very rare procedure, lung transplants and heart-lung transplants are more common alternatives.Pulmonary Hypertension Research Paper
How to Treat Pulmonary Hypertension: Groups 2 and 3
Group 3 pulmonary hypertension includes cases of the disease caused by left-side diseases such as mitral valve disease. In order to treat patients in this group, physicians will focus on the treatment of the underlying condition with lifestyle changes, medicines, and surgery.
Similarly, cases in the group 3 pulmonary hypertension are caused by lung conditions like chronic obstructive pulmonary disease (COPD) and interstitial lung disease, or sleep disorders like sleep apnea. In addition to treating the underlying cause of the disease, physicians may also recommend oxygen therapy, a resource administrated through soft, plastic prongs that fir into the nose at home or in a hospital, to increase the level of oxygen in the blood.
How to Treat Pulmonary Hypertension: Groups 4 and 5
Group 4 pulmonary hypertension includes cases of the disease caused by blood clots in the lungs or blood clotting disorders. To treat this, patients are often prescribed blood-thinning medicines to prevent the formation or enlargement of clots. Surgery is also an option to remove scarring in the pulmonary arteries due to old blood clots. Group 5 pulmonary hypertension includes all other conditions that cause PH, such as thyroid disease and sarcoidosis, or an object, such as a tumor pressing on the pulmonary arteries. The treatment of patients in this group is conducted by treating the underlying cause.Pulmonary Hypertension Research Paper
Treatments Used in All Types of Pulmonary Hypertension
In addition to the personalized treatments for each group, there are also numerous treatments that can be applied to all types of pulmonary hypertension. These include diuretics, or water pills, which help reduce fluid buildup in the body, such as swelling in the ankles or feet. Blood-thinning medicines are used to avoid blood clots, while digoxin improves heart beat strength, helping it pump more blood, as well as to control the heart rate in the case of abnormal heart rhythms, such as atrial fibrillation or atrial flutter.
Physicians may also recommend oxygen therapy to increase the levels of oxygen in the blood, as well as lifestyle alterations and moderated physical activity to improve patients ability to be active. Researchers worldwide are currently working to improve pulmonary hypertension treatments, and find a cure for the disease.
Pulmonary Hypertension Often Missed in its Early Stages
With advances in diagnosis and treatment options, pulmonary hypertension is more treatable today than ever before. The biggest challenge, says Ronald Zolty, MD, cardiologist at Nebraska Medicine, is getting an early diagnosis.
"Pulmonary hypertension in its earliest stages is difficult to diagnose and often gets overlooked because it doesn’t show up in standard cardiac diagnostic tests," says Dr. Zolty.
In its earliest stages, patients often complain of shortness of breath, especially with exertion. If an echo cardiogram is ordered, it too will typically come out normal unless the right side of the heart is evaluated. Even then, the test may still appear normal if the patient is in his or her earliest stages.Pulmonary Hypertension Research Paper
"At Nebraska Medicine, we perform a comprehensive evaluation to determine if the patient has pulmonary hypertension and to find the source or cause of the condition," says Dr. Zolty. "Knowing the cause of this condition is extremely important as this will guide us in how to appropriately treat the patient.
"The earlier we diagnose this disease, the more successful we will be at stopping its progression. If nothing is done to treat it, it will continue to progress. As the disease progresses, the patient will begin to develop resting pulmonary hypertension and eventually, right side heart failure. However, when the disease is caught early and treated appropriately, many patients can go on to live a normal lifespan."
Early symptoms of pulmonary hypertension include shortness of breath with exertion followed by fatigue, lower extremity edema and abdominal distention. In more advanced stages of the disease, the patient may experience dizziness and syncope.
"We like to see patients when they are having shortness of breath with exertion," says Dr. Zolty. All patients will undergo a comprehensive evaluation process that starts with a left and right side echo cardiogram. This is followed by a B-type Natriueretic Peptide (BNP) blood test to measure the level of fluid retention and heart stretch. These two tests may be negative if the patient is in the earlier stages of the disease. The next test performed is a right side cardiac catheterization – the gold standard test for pulmonary hypertension. The catheter is placed in the patient’s jugular vein to assess resting cardiac and pulmonary pressures. The patient is then asked to exercise for three minutes to see if exercise induces elevation of the pulmonary pressures which may explain why the patient is experiencing shortness of breath with exertion. If pulmonary hypertension is confirmed, a host of other tests are performed to determine the cause. These may include a sleep study, pulmonary function tests, perfusion ventilation nuclear tests, blood work, liver function test, connective tissue tests, HIV test and a cardiac MRI.Pulmonary Hypertension Research Paper
"We like to follow up with patients about six weeks later with an echo cardiogram to make sure their medications are working properly," says Dr. Zolty. "Once we have feel like we have them on the right treatment plan, we recommend follow up every three months to ensure the medications are keeping the condition under control."
"Eighty percent of patients have very good results," says Dr. Zolty. "About 5 to 10 percent, of patients may not respond to oral therapy and may need to be placed on continuous par enteral (intravenous or subcutaneous) therapy or may even be considered for lung or combined heart and lung transplantation. Nebraska Medicine has both a heart and lung transplant program, which can evaluate the patient for a transplant.
There are a number of conditions that can cause pulmonary hypertension. In some cases, it may be idiopathic or familial. The most common cause of pulmonary hypertension is heart failure or other types of heart disease like diastolic heart disease or valvular disease. This is followed by lung diseases like emphysema, bronchitis or pulmonary fibrosis; autoimmune diseases like lupus, scleroderma and rheumatoid arthritis; cirrhosis of the liver, HIV, illegal drug use, congenital heart defects; pulmonary embolism; and diseases like sickle cell anemia and sarcoidosis.
Pulmonary hypertension is more common in men ages 50 and over but it is also seen in young women as early as their 20s or 30s due to genetics, congenital heart defects and connective tissue diseases like sclerodermia.
"This is a disease that affects about 3 percent of the population, but its prevalence is increasing as we see an increase in heart disease," says Dr. Zolty.
Pulmonary arterial hypertension (PAH) is a rapidly progressive disease, ultimately leading to right heart failure and death. Accumulating evidence indicates that intervention early in disease progression results in better outcomes than delaying treatment.Pulmonary Hypertension Research Paper
In this review we will discuss the assessments and strategies that can be used to monitor disease progression and guide clinical management. Many tools, such as symptoms, functional classification, exercise capacity, haemodynamic measures, findings on cardiac imaging and levels of bio markers, have shown to be prognostic for survival both at diagnosis and during treatment. However, attempts to define goal thresholds have produced a variety of results.
Several groups have developed risk calculators to estimate individual patient's mortality risk, but the accuracy of these tools across different patient populations remains unknown. What is clear is the importance of regularly assessing a range of parameters and then tailoring treatment goals to each patient. In addition, the use of a multidisciplinary team approach is crucial in order to support patients through all aspects of managing their condition.
There is still an urgent need for prospective collaborative initiatives to assess novel goals and improve treatment strategies that would allow physicians to personalize and optimize clinical management for their patients with PAH.Pulmonary Hypertension Research Paper
Pulmonary hypertension is a chronic and progressive disease characterized by high blood pressure in the pulmonary arteries, the blood vessels of the lungs.
There are many potential causes of the disease that, along with how early the disease is diagnosed and when treatment is started in the patient, can affect prognosis.
There is currently no known cure for pulmonary hypertension, but research is ongoing, and with the continual improvement of diagnostic techniques and therapies, it is becoming possible to diagnose the disease earlier to manage the symptoms for longer.
Pulmonary hypertension is a progressive disease, which means it worsens over time, although the speed varies based on the individual and the class of pulmonary hypertension. If left untreated, the prognosis is poor and the disease is often fatal within a few years, emphasizing the need for a quick and accurate diagnosis.
Life expectancy
The survival of patients with pulmonary hypertension used to be around three to five years, and it could take two or more years to correctly diagnose. But the life expectancy of patients with pulmonary hypertension has improved dramatically since the disease was first identified in 1891. This is because of the continual improvement of diagnostic techniques and the development of specialized therapies for pulmonary hypertension, beginning with the introduction of Flolan (epoprostenol GM) in 1995.
Improved diagnostic techniques result in faster and more accurate diagnoses, which then results in treatment beginning at earlier stages of the disease. Early treatment can significantly improve a patient’s quality of life and can improve the overall life expectancy.
For example, a study observing more than 1,000 patients with pulmonary hypertension in Taiwan determined that 62.6 percent of patients were now surviving 10 years or more after diagnosis. Researchers concluded that the mortality rate of patients with pulmonary hypertension was more than three times higher than in the control group of healthy people. Pulmonary Hypertension Research Paper
ORDER A PLAGIARISM-FREE PAPER HERE
Prognostic factors
There is currently no exact method of accurately predicting prognosis following a diagnosis of pulmonary hypertension. However, there are some known risk factors associated with a better or worse outcome.
Potential indicators of a poorer prognosis include:
- A higher functional classification at diagnosis, which indicates a later stage of the disease.
- Comorbidities, or the presence of additional conditions, such as diabetes.
- Presence of pericardial effusion, or abnormal accumulation of fluid around the heart.
Some types of pulmonary hypertension, such as scleroderma-associated pulmonary arterial hypertension and chronic obstructive pulmonary disease (COPD), are also associated with a poorer life expectancy.
Prognosis of group 4 pulmonary hypertension
Group 4 pulmonary hypertension, or chronic thromboembolic pulmonary hypertension (CTEPH), is the only type of pulmonary hypertension that can be cured. CTEPH is caused by blood clots in the pulmonary arteries, and many patients are able to undergo a surgical procedure, called pulmonary thromboendarterectomy (PTE) to remove these clots. Around 85 to 90 percent of patients will experience significantly fewer or no symptoms of CTEPH following the procedure.Pulmonary Hypertension Research Paper
Pulmonary hypertension (PH) is a rare but severe lung disease in which patients experience high blood pressure in the lungs. The disorder affects the pulmonary arteries, which are the blood vessels responsible for transporting blood from the heart to the lungs. As the pulmonary arteries become narrowed and thickened, the heart needs to work harder to properly pump the blood through the right heart ventricle, which can result in enlargement and weakening of the heart, right heart failure, and death.
There are different causes of pulmonary hypertension, but not all of them are fully understood. The most common symptoms include shortness of breath (dyspnea), fatigue, dizziness or fainting spells (syncope), pressure or pain in the chest, swelling (edema) in the ankles, legs and abdomen (ascites), a bluish color in the lips and skin (cyanosis) and irregular heart beat. Pulmonary hypertension lifespan and survival depend on numerous factors and is not exact.
Prognosis After Pulmonary Hypertension Diagnosis
Pulmonary hypertension is a progressive disease, which means that it worsens as time advances, quickly or slowly depending on the patient and characteristics of the disease. There is currently no cure for the disease, but treatments exist to help ease symptoms and prolong lifespan. When untreated, pulmonary patients face a poor prognosis, estimated at 2.8 years. The probability of survival for untreated patients is 68% f0r one year after the onset of the disease, which drops to 48% after three years and to 34% after five years, according to the Ohio State University Lung Center.Pulmonary Hypertension Research Paper
But recent research demonstrates that pulmonary hypertension lifespan has increased to an average of seven years. The most common reasons for pulmonary hypertension-related deaths are right heart failure or congestive heart failure, severe bronchitis, autoimmune diseases, congenital malformations, chronic lower respiratory disease, and emphysema.
Evolution Of Pulmonary Hypertension Lifespan
Pulmonary hypertension was first diagnosed in 1891, but it was not until 1994 that the first treatment for the disease was discovered. When the medication Flolan was commercialized, it meant more encouraging outcomes for patients with pulmonary hypertension. Previous to the launch of the drug, patients would succumb to the disease about three years after onset. Diagnosis took an average of two years.
The development of new drugs to treat pulmonary hypertension resulted in an immediate increase of lifespan to about five years and later to seven years. It also brought improved of quality of life. During the past 20 years, the outlook of pulmonary hypertension has gone from no treatments at all to more than 10 approved medications. Patients who undergo lung transplant also face better prospects. But some factors negatively impact the disease.Pulmonary Hypertension Research Paper
Factors That Impact Pulmonary Hypertension Lifespan
Pulmonary hypertension lifespan, treatment and survival is closely related to the subtype and stage of disease.
The study “Prognostic Factors in Pulmonary Hypertension” analyzed variables that influence the progress of PH and demonstrated that despite the greater prevalence of the disease among women, gender does not impact survival.
On the other hand, age is an important factor for survival. The average age at death is 64.72 years.
Almost 7% of the patients in the study developed congenital heart defects. Suffering from other conditions is known to increase mortality and reduce quality of life.
The study indicated a higher mortality among patients with idiopathic pulmonary hypertension (when the cause of the disease is not known), over primary or secondary pulmonary hypertension. Proper treatment that focuses on the underlying cause of the disease largely improves lifespan.
A sedentary lifestyle, living in high altitudes and being pregnant typically impact the health of the heart and lung which affects pulmonary hypertension lifespan.Pulmonary Hypertension Research Paper
Drugs for pulmonary hypertension
A number of different drugs are used to treat pulmonary hypertension, sometimes in combination.
- Diuretics are used to reduce fluid retention and swelling. They are also known as water pills.
- Digoxin is used to treat heart failure. It helps to control the heart rate and rhythm, and it increases the amount of blood pumped by each heartbeat.
- Blood-thinning drugs, such as warfarin, can help to prevent blood clots. These are more likely in people with pulmonary hypertension.
- Calcium-channel blockers, such as diltiazem, may help some patients.
- Phosphodiesterase-5 (PDE5) inhibitors increase the blood flow by widening blood vessels. This is called vasodilation. Sildenafil is an example of a PDE5 inhibitor.
- Endothelin receptor antagonists, such as bosentan and ambrisentan, limit the constriction of arteries that can happen when a person has too much natural peptide.Pulmonary Hypertension Research Paper
Surgical solutions
More invasive treatments are also possible in cases where medicine is not having the desired effect.
These include:
- Atrial septostomy: The surgeon introduces a shunt between heart chambers and improve cardiac output while the patient awaits transplant surgery.
- Lung transplant: This is a procedure to replace one lung or both lungs.
- A combined heart and lung transplant: This procedure is an intensive double transplant.
Chronic thromboembolic pulmonary hypertension is a presentation of high blood pressure in the lungs that involves a number of blood clots in the arteries.
Some patients with chronic thromboembolic pulmonary hypertension may undergo a procedure called a pulmonary thromboendarterectomy (PTE). This is specialized heart surgery to remove blood clots from coronary arteries.
Continuous oxygen therapy may be necessary to help maintain oxygen saturation in the blood, especially in a patient who also has lung disease.
During a high-altitude flight, a patient may need oxygen therapy to compensate for reduced oxygen levels.
Pulmonary hypertension has no cure. However, treatment can ease symptoms and slow the development of the condition.
What is primary pulmonary hypertension?
Primary pulmonary hypertension (PPH) is high blood pressure in the lungs. It is also known as idiopathic pulmonary arterial hypertension. It’s a rare lung disorder in which the blood vessels in the lungs narrow (constrict) and the pressure in the pulmonary artery rises far above normal levels. The pulmonary arteries carry blood from your body to the lungs, where carbon dioxide is traded for oxygen.Pulmonary Hypertension Research Paper
Pulmonary hypertension is a serious, ongoing (chronic) disease. It can lead to heart failure if it’s not treated.
What causes primary pulmonary hypertension?
Experts don't know what causes primary pulmonary hypertension. Often there is no underlying heart or lung disease causing the high blood pressure.
Some forms of pulmonary hypertension are linked to a gene defect that can run in families. Researchers believe this gene mutation makes the blood vessels more sensitive to certain factors. They believe the blood vessels narrow when exposed to these factors.
What are the symptoms of primary pulmonary hypertension?
Each person's symptoms may vary. Symptoms can develop so slowly that you can have it for years without knowing it. Symptoms may include:
- Bluish lips and skin
- Chest pain (angina)
- Dizziness
- Dry cough
- Extreme tiredness (fatigue)
- Fainting
- Feeling like your heart is fluttering or beating fast or hard (palpitations)
- Racing pulse
- Swelling in the ankles or legs
- Trouble breathing or shortness of breath, especially with activity
- Trouble getting enough air
These symptoms get worse as the disease progresses. More severe symptoms are a sign of more advanced disease. In advanced stages, you may:
- Have symptoms even when resting
- May become bedridden
The symptoms of PPH looks like other conditions or health problems. This condition can be hard to diagnose. Many people ignore symptoms because they think they are simply out of shape. If you or a family member have any of these symptoms, talk with your healthcare provider for a diagnosis.Pulmonary Hypertension Research Paper
How is primary pulmonary hypertension diagnosed?
PPH is rarely discovered in a routine health exam. In its later stages, the signs of the disease can be confused with other conditions affecting the heart and lungs.
It may be diagnosed when other diseases are ruled out. Tests may include:
- Chest X-ray. A test that takes pictures of internal tissues, including the heart.
- ECG. This test records the strength and timing of the electrical activity of the heart. It shows abnormal rhythms and can sometimes find heart muscle damage. Small sensors are taped to your skin to pick up the electrical activity.
- Echo cardiogram. This test uses sound waves to check the heart’s chambers and valves. The echo sound waves create a picture on a screen as an ultrasound probe (transducer) is passed over the skin over the heart. This test can show heart damage and enlargement.
- Pulmonary function tests. These are diagnostic tests that help to measure the lungs’ ability to move air into and out of the lungs. The tests are often done with special machines you breathe into.
- Perfusion lung scan. This is a type of nuclear radiology test. A small amount of a radioactive substance is used to help find changes in the arteries leading to the lungs and blood flow within the lungs. This scan can also be used to check lung function.
- Cardiac catheterization of the right side of the heart. In this test, the doctor passes a hollow tube through a large tube (catheter) in the vein. He threads the tube through the right side of the heart and into the pulmonary artery. This is the only test that directly measures the pressure inside the pulmonary arteries.Pulmonary Hypertension Research Paper
- Blood tests. These can be used to check the oxygen levels in the blood, assess liver and kidney function, and look for other diseases. Certain blood tests can also help to check strain on the heart.
How is primary pulmonary hypertension treated?
There is no cure for primary pulmonary hypertension. Treatment tries to manage symptoms and may include 1 or more of the following:
Medicines
- Anticoagulants. These are blood thinners used to make the blood less likely to clot and help it flow more freely.
- Diuretics. Called water pills, these are used to decrease the amount of fluid in the body. They help reduce swelling and the amount of work the heart has to do.
- Calcium channel blocking or vasodilator medicines. These are used to improve the heart’s ability to pump blood.
- Pulmonary artery specific therapy. This type of medicine targets the pulmonary arteries and tries to decrease the pressure of the blood flow through these arteries. These medicines include ambrisentan, sildenafil, and epoprostenol.
- Other medicines. These are used to help lower blood pressure in the lungs. They also help the heart beat stronger and pump more blood.
Oxygen therapy
Some people also need supplemental oxygen delivered through nasal prongs or a mask if breathing becomes difficult.
Lung or heart-lung transplant
This may be a choice for people with severe disease.
Staying healthy
The condition can be made worse by a number of factors. You can do certain things that will help you stay as healthy as possible. To keep a healthy lifestyle with primary pulmonary hypertension:
- Don’t smoke.
- Try to stay away from high altitudes and travel in non pressurized airplane cabins. Consider using supplemental oxygen during air travel.
- Before starting an exercise program, ask your healthcare provider about the type and amount of physical activity that is safe for you.
- Don’t participate in activities that can lead to dangerous symptoms, such as chest pain or dizziness.
- Be careful when using both prescription and over-the-counter medicines. Ask your physician or pharmacist which medicines are safe for a person with PPH.
- Pregnancy and childbirth can pose serious dangers to women with this condition. Talk with your healthcare provider if you are thinking about getting pregnant.
- Consider getting a pneumococcal pneumonia vaccine and yearly flu vaccines. Flu and pneumonia can be very dangerous for people with this condition. Pulmonary Hypertension Research Paper
Key points about primary pulmonary hypertension
- Primary pulmonary hypertension (PPH) is a rare lung disorder that causes high blood pressure in the lungs.
- Experts don't know what causes it.
- Symptoms can develop so slowly that you can have the condition for years without knowing it. And symptoms get worse as the disease progresses.
-
Pulmonary hypertension is a serious, ongoing (chronic) disease. It can lead to heart failure if it’s not treated.
- There is no cure for the condition. Treatment is aimed at managing symptoms.
Pulmonary arterial hypertension is defined as a mean pulmonary arterial pressure greater than 25 mm Hg at rest or 30 mm Hg during physical activity. Pulmonary arterial hypertension is classified into subgroups, including idiopathic, heritable, and pulmonary arterial hypertension associated with other conditions. A detailed history, thorough physical examination, and most importantly, a high index of suspicion are essential to diagnosis. Evaluation includes electrocardiography and exclusion of other causes of symptoms. Targeted laboratory testing can help identify the subgroup of pulmonary arterial hypertension. Right heart catheterization is required to confirm the diagnosis. Standard treatment options include oral anti coagulation, diuretics, oxygen supplementation, and for a small percentage of patients, calcium channel blockers. Newer treatments include prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase type 5 inhibitors. Combination therapy has been shown to improve pulmonary arterial pressure, but more research is needed. Intervention al procedures for patients with pulmonary arterial hypertension include balloon atrial septostomy and lung transplantation.Pulmonary Hypertension Research Paper
Pulmonary arterial hypertension (PAH) is a rare, under diagnosed condition defined as elevation of mean pulmonary arterial pressure. In patients with PAH, the average pulmonary arterial pressure is greater than 25 mm Hg at rest (compared with 15 mm Hg in patients without PAH) or 30 mm Hg during physical activity, as measured by right heart catheterization. The prevalence of PAH varies among specific populations, but one study estimated that it affects 15 in 1 million adults.1 Idiopathic PAH occurs mainly in persons in their 20s and 30s, with an overall female-to-male ratio of 1.7:1, which is higher in black persons (4.3:1).2 Risk factors for PAH include a family history of PAH, congenital heart disease, connective tissue disease, portal hypertension, sickle cell disease, thyroid disease, human immunodeficiency virus (HIV), and use of certain drugs and toxins. Table 1 lists the clinical classification of PAH, which was updated in 2008.
Pulmonary Hypertension is a term to describe a rare disease in which the blood pressure in the lungs (pulmonary artery system) is higher than normal. The staff of the Adolescent and Adult Congenital Heart Disease Program at Nationwide Children's Hospital is dedicated to providing advanced therapy for this condition.
Pulmonary Hypertension is a term to describe a rare disease in which the blood pressure in the lungs (pulmonary artery system) is higher than normal. The blood pressure that is measured on your arm by a cuff reflects systemic or your body’s blood pressure. Normal systemic blood pressure is 120/80 mmHg. Normal blood pressure within the lungs is much lower and much more difficult to evaluate. Normal blood pressure in the lungs is 15 -25 mmHg, or about 1/5th the bodies blood pressure.Pulmonary Hypertension Research Paper
Pulmonary Hypertension results when the blood vessels constrict (tightens). Over time this constriction causes fibrosis (scars) of the vessel and higher pulmonary blood pressure. The chambers on the right side of the heart (right atrium and right ventricle) have difficulty pumping blood out to the pulmonary artery and through the lungs. The strain on the heart to overcome this high pressure and constriction causes the heart to become enlarged and weak. Eventually the heart cannot keep up with the body’s demands. This is known as heart failure.
Pulmonary Hypertension can be classified into two groups:
- Idiopathic or Primary Pulmonary Hypertension - Pulmonary Arterial Hypertension (PAH) that is not the result of another medical condition. This means that your doctor may not be able to explain to you why you or your child may have developed pulmonary hypertension. Although idiopathic pulmonary hypertension affects men, women and children it is most common in women between the ages of 20-45 years of age. It is possible that there is a family or hereditary link associated with the disease. It is also believed that the use of certain drugs such as diet pills (Redux, Fen-phen), street drugs like cocaine or amphetamines and disease such as AIDS and liver disease may trigger the disease.Pulmonary Hypertension Research Paper
- Secondary Pulmonary Hypertension - Pulmonary Hypertension that is associated with or the result of another medical condition.
Signs and Symptoms of Pulmonary Hypertension
The signs and symptoms of Pulmonary Hypertension include:
- Fatigue
- Shortness of Breath
- Chest Pain
- Dizziness
- Fainting (syncope)
- Swollen ankles and legs (edema)
- Swelling in abdomen (ascities)
- Rapid pulse or palpitations of the heart
Conditions that Cause Pulmonary Hypertension
There are many diseases that can cause pulmonary hypertension (PH). The following is a brief explanation of each of these conditions.
PH Associated with Connective Tissue Diseases
Connective Tissue Diseases such as scleroderma, CREST syndrome, rheumatoid arthritis, and systemic lupus are autoimmune disease associated with pulmonary hypertension. Of these conditions scleroderma is the most common disease link to pulmonary hypertension.
PH Associated with Hypoxemia (Low Oxygen)
Oxygen opens the lung passages. When the body is deprived of oxygen it can cause constriction of the lung vessels resulting in pulmonary hypertension. Diseases that affect lung breathing passages and decrease oxygen include asthma, emphysema, chronic bronchitis, interstitial lung disease and cystic fibrosis.Pulmonary Hypertension Research Paper
Another form of lung disease related to low oxygen and periods of not breathing (apnea) during the sleep cycle – is called sleep apnea. Obstructive Sleep Apnea (the inability to breath due to blocked airway passage) is the most common form found in overweight middle aged adults. Treatment with breathing machines (CPAP/Bi Pap) during sleep helps improve oxygen levels.
PH Associated with Congenital Heart Disease
A child may be born with a hole in the septum of the heart. The septum is the wall that separates the right and left side of the heart.
If the hole is between the two upper chambers, it is called atrial septal defect (ASD). Most ASD’s are repaired during childhood; however, it is possible to repair these holes at any age if there is little to no signs of pulmonary hypertension that exists.
If the hole is between the two lower chambers it is called a ventricular septal defect. (VSD). Ventricular septal defects are the most common congenital heart defects. When a defect is present, blood can flow across the hole from the left side of the heart to the right. Children born with VSD’s are more likely to develop pulmonary hypertension than those with ASD’s if they are not closed early in life. The reason is because there is excessive blood flow and pressure through the hole into the right side of the heart and lungs that results in enlargement of both the right atrium and ventricle. Over time the extra blood flow into the lungs causes damage to the blood vessels resulting in pulmonary hypertension.Pulmonary Hypertension Research Paper
PH Associated with Left Ventricular Diastolic Dysfunction
The heart cycle is divided into two phases, systole and diastole. Systole is when the heart is pumping blood out to the lungs and body. After the ventricles eject the blood they must relax and refill with blood to prepare again for pumping. This relaxation phase is known as diastole. The ventricles can become stiff over time not allowing the ventricles to fill completely with blood during diastole. The stiffness of the ventricles and inability to relax causes the pressure to rise on the left side of the heart, and eventually the pressure in the lungs rises. This condition is known as diastolic dysfunction. Diastolic dysfunction may occur with normal aging but is also associated with chronic high blood pressure, coronary artery disease (blockage of the coronary arteries) and many forms of cardiomyopathies (failure of the heart muscle). Pulmonary Hypertension Research Paper
Diastolic dysfunction can only be diagnosed by heart catheterization. The data that the doctor obtains during the heart catheterization will help identify this type of heart disease. Although diastolic dysfunction is a form of pulmonary hypertension the treatment is different and the goal is to relax the left ventricle using specific drugs such as nitrates. It is also important to control the body’s (systemic) blood pressure, treat coronary artery disease and control lung congestion with diuretics.
PH Associated with Chronic Thromboembolic/Embolic Disease
A thrombus or thromboembolism is a blood clot that blocks the passage of blood through a vessel. If blood clots travel to the lung, the obstruction may lead to pulmonary hypertension. Sometimes blood clots in the lungs do not cause symptoms. Pulmonary Hypertension caused by blood clots is rare and may require surgical removal of the clots by a procedure called thromboendarterectomy.
There are many diseases that can cause pulmonary hypertension (PH). The following is a brief explanation of each of these conditions.
How is Pulmonary Hypertension Diagnosed?
Testing for pulmonary hypertension includes:
- A complete history and physical exam.
- An electrocardiogram (ECG) may show a strain on the right side of your heart
- Blood Tests to evaluate if you have any form of collagen vascular disease
- A chest CT Angiogram to assess for lung disease and detect blood clots in the lung circulation
- A pulmonary function test to measure lung capacity ( how much air the lungs inhale and exhale). Poor lung capacity reflects the degree of damage or deterioration of the lungs.
- An exercise test called a six minute walk. You will be required to walk on a flat surface as fast as you can for six minutes to evaluate how much exercise you can do before you have symptoms.Pulmonary Hypertension Research Paper
- An echo cardiogram and cardiac catheterization
The echo cardiogram can demonstrate the pump function of the heart and the quality of blood flow through the heart valves. Although this is a good test it is not the most accurate or reliable test for the diagnosis of pulmonary hypertension.
The only precise way to diagnose pulmonary hypertension is with a cardiac catheterization. A cardiac catheterization reveals important information including:
- How well the heart is working (known as cardiac output)
- How high the pressures are within the pulmonary artery (mean pulmonary artery pressure)
- How stiff or tight the pulmonary blood vessels are (known as pulmonary vascular resistance)
- How well medicines are working
Patients living with Pulmonary Hypertension have several treatment options to improve their quality of life.
Treatment Options
Nationwide Children's Hospital is dedicated to providing advanced therapy for pulmonary hypertension. Patients living with pulmonary hypertension have several treatment options to improve symptoms of the disease and their quality of life, available therapies include:
- Intravenous Flolan
- Intravenous Remodulin
- Subcutaneous Remodulin
- Endothelin Antagonists: Tracleer (Bosentan)/Sitaxsentan (Thelin)/Ambrisentan
- Phosphodiesterase type 5 inhibitor: Viagra (Sildenafil)
- Inhaled Iloprost (Ventavis)
- Clinical Research of new medications
- Lung transplant or Combined Heart/Lung transplant
Pulmonary arterial hypertension (PAH) is a rare, progressive disorder characterized by high blood pressure (hypertension) in the arteries of the lungs (pulmonary artery) for no apparent reason. The pulmonary arteries are the blood vessels that carry blood from the right side of the heart through the lungs. Symptoms of PAH include shortness of breath (dyspnea) especially during exercise, chest pain, and fainting episodes. The exact cause of PAH is unknown and although treatable, there is no known cure for the disease. PAH usually affects women between the ages of 30-60. Individuals with PAH may go years without a diagnosis, either because their symptoms are mild, nonspecific, or only present during demanding exercise. However, it is important to treat PAH because without treatment, high blood pressure in the lungs causes the right heart to work much harder, and over time, this heart muscle may weaken or fail. The progressive nature of this disease means that an individual may experience only mild symptoms at first, but will eventually require treatment and medical care to maintain a reasonable quality of life.Pulmonary Hypertension Research Paper
Approximately 15-20% of patients with PAH have heritable forms of PAH. People with heritable PAH have either: (1) an autosomal dominant genetic condition associated with mutations in the BMPR2 gene or other recently identified genes now associated with HPAH or other forms of PAH or associated conditions such as pulmonary capillary hemangiomatosis or pulmonary veno-occlusive disease, or (2) are members of a family in which PAH is known to occur as primary disease.
Introduction
The first reported case of PAH occurred in 1891, when the German doctor E. Romberg published a description of a patient who, at autopsy, showed thickening of the pulmonary artery but no heart or lung disease that might have caused the condition. In 1951, 3 cases were reported by Dr. D.T. Dresdale in the U.S. and the illness was originally called primary pulmonary hypertension. PAH has been linked to diet drugs such as Fen-Phen, Pondimin and Redux. These drugs were taken off the market in 1997, although cases related to drugs and toxins, such as methamphetamines do still appear. PAH is also associated with a number of other medical diseases such as cirrhosis and connective tissue diseases like scleroderma. About 30% of patients with PAH have an associated connective tissue disease.
Signs & Symptoms
PAH symptoms are those that are usually due to not having enough oxygen in the blood. In most cases, the initial symptom is severe shortness of breath following exertion. Additional symptoms include excessive fatigue, weakness, chest pain, dizzy spells, and fainting episodes.Pulmonary Hypertension Research Paper
Affected individuals may also have a cough, sometimes with blood (hemoptysis), an enlarged heart and liver, low blood pressure (hypotension), and hoarseness due to compression of a nerve in the chest by an enlarged pulmonary artery.
Some affected individuals may experience puffiness or swelling of the face, ankles, abdomen and feet due to abnormal accumulation of fluid (edema) within fascial tissues.
Individuals with advanced stages of PAH may have abnormal bluish discoloration of the skin due to low levels of circulating oxygen in the blood (cyanosis). In addition, in severe cases of PAH, the right chamber (ventricle) of the heart is abnormally enlarged (hypertrophy), resulting in diminished functioning of the right portion of the heart and, potentially, right heart failure. Some patients with PAH do not seek medical advice until they are no longer able to continue with their normal activities. At this time, the disease may have progressed to a point where the patient is completely bedridden from shortness or breath or other symptoms.
Causes
The exact cause of PAH is unknown. Researchers believe that injury to the layer of cells that line the small blood vessels of the lung, perhaps then causing or in concert with changes in the smooth muscle cells in the vessel wall, initiates blood vessel disease. This injury, which occurs for unknown reasons, results in the contraction of smooth muscle and therefore narrows the vessel. Researchers also think that most people who develop PAH have blood vessels that are particularly sensitive to certain internal or external factors and constrict, or narrow, when exposed to these factors.Pulmonary Hypertension Research Paper
Approximately 15-20% of patients with PAH have heritable PAH. Heritable PAH is an autosomal dominant genetic condition caused by mutations in the BMPR2 gene most commonly, though recently other genes and pathways have been identified. In approximately 20% of families with PAH, we do not yet know the underlying gene mutations.
Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary for the appearance of the disease. The abnormal gene can be inherited from either parent, or can be the result of a new mutation in the affected individual. Approximately 80% of individuals who have a mutated (abnormal) BMPR2 gene will not develop PAH, so other genes or environmental triggers must be necessary for PAH to develop. The risk of passing the abnormal gene from parent to offspring is 50% for each pregnancy and the risk is the same for males and females.
Of note, there now exist several publications associating PAH with mutations in other genes in a small number of patients (e.g. CAV1, KCNK3, etc), although many of those genes are closely linked to BMPR2 in terms of biologic signaling (SMAD9, ALK1, endoglin). Recently, pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis have been linked to mutations in the gene EIF2AK4. The function of this gene is still being studied.Pulmonary Hypertension Research Paper
In August 1996, the Food and Drug Administration (FDA) evaluated data from a report of the International Primary Pulmonary Hypertension Study (IPPHS). The study examined the relationship between appetite-suppressant drugs (dexfenfluramine [Redux] and fenfluramine [Pondimin] and what was then called PPH. Findings indicated that the risk of PPH (now called a type of PAH) in individuals using appetite-suppressant drugs for three months or longer is about nine times higher than the risk for non-users. The final IPPHS report estimated that the risk of this disorder is about 23 times higher in individuals who use appetite-suppressants for three months or longer. These drugs were taken off the market in 1997, though other diet drugs have been associated with PAH such as benfluorex that was used in Europe until 2009.
Along with the increased risk of diet pills, other exposures have been associated with the development of PAH. These include methamphetamines and dasatanib. In addition, a very small percentage of HIV patients with AIDS develop PAH that is identical in presentation to primary PAH. In terms of other exposures which may contribute to the development of PAH, few are validated in rigorous studies. However, female sex hormones are an area of great interest for several reasons, including: (1) the higher risk of PAH among females and (2) the association of pregnancy with the development of PAH (may be more common in the peripartum period), and (3) some association with exogenous estrogen intake the development of PAH.Pulmonary Hypertension Research Paper
Several conditions have been associated with PAH such as liver disease (cirrhosis), congenital heart disease and connective tissue diseases such as scleroderma. The mechanisms through which these conditions might cause PAH are presently being studied and are unknown.
Scleroderma is a chronic systemic autoimmune disease (primarily of the skin) characterized by fibrosis (or hardening), vascular alterations, and auto-antibodies. One of the serious complications of this rare disease is PAH, which can occur in up to a third of scleroderma patients. Almost everyone with scleroderma experiences Raynaud’s phenomenon as well. (For more information on this disorder, choose “scleroderma” as your search term in the Rare Disease Database.)
Human Immunodeficiency Virus (HIV) infection can also affect the pulmonary blood vessels and put a strain on the heart, typically in the setting of overt AIDS due to HIV. HIV is a rare virus which causes AIDS, a chronic and life-threatening illness. HIV lowers the immune system and makes the body much more susceptible towards disease. Symptoms of HIV are at first, similar to those of the flu, and may include fever, swollen glands, headache, sore throat, and a rash.
Persistent pulmonary hypertension of the newborn (PPHN) is a kind of PAH that occurs when a newborn’s circulatory system does not adapt to breathing outside the womb. It occurs most often in full-term or post-term babies who had a difficult birth. Newborns that have PPHN have rapid respiration (tachypnea) and abnormal bluish discoloration of the skin due to low levels of circulating oxygen in the blood (cyanosis). The disorder is believed to be caused by insufficient oxygen in the blood flowing to the lungs just before, during or after birth (perinatal hypoxemia), although its precise cause is unknown.Pulmonary Hypertension Research Paper
Affected Populations
PAH occurs 3-5 times more frequently in females as in males. It tends to affect females between the ages of 30 and 60. New cases are estimated to occur in one to two individuals per million each year in the U.S. The incidence is estimated to be similar in Europe. Approximately 500-1000 new cases of PAH are diagnosed each year in the U.S. There is no ethnic or racial group that is known to have a higher frequency of patients with PAH. An exception to this is an apparent paucity of cases of HPAH among subjects of African ancestry, although this may relate to reporting bias and has not been rigorously studied.
A rare form of pulmonary hypertension affects individuals who are at high altitude levels (e.g., mountain climbing). It is not recommended for people with PAH or a family history of PAH to live at high altitudes.
Diagnosis
It can often be hard to detect PAH in a routine clinical examination, even if the disease has progressed. Symptoms of PAH are not unique and may be confused with many other diseases that cause a lack of oxygen in the blood. The diagnosis of PAH is also one of exclusion, meaning that PAH is only diagnosed when other causes of pulmonary hypertension have been ruled out and there seems to be no known cause of the hypertension. The tests that are commonly performed to diagnose PAH and rule out other diseases are echocardiography, blood tests, pulmonary function tests, X-rays of the chest, electrocardiography (ECG), and the “6-minute walk test”, which essentially measures how far an individual can walk in that time period. Ultimately, the majority of subjects undergo confirmation by cardiac catheterization with and without vasodilator testing.
Heritable PAH is confirmed if two or more family members have PAH or if a BMPR2 gene mutation or mutation in another gene known to cause PAH is identified in the affected person. Molecular genetic testing is available for mutations in the BMPR2 gene, but should only be performed in concert with genetic counseling.Pulmonary Hypertension Research Paper