Monitoring Fetal Growth Research Paper
Globally, approximately 140 million births occur every year (1). The majority of these are vaginal births among pregnant women with no identified risk factors for complications, either for themselves or their babies, at the onset of labor (2, 3). However, in situations where complications arise during labor, the risk of serious morbidity and death increases for both the woman and baby. Over a third of maternal deaths and a substantial proportion of pregnancy-related life-threatening conditions are attributed to complications that arise during labor, childbirth or the immediate postpartum period, often as result of hemorrhage, obstructed labor or sepsis (4, 5). Similarly, approximately half of all stillbirths and a quarter of neonatal deaths result from complications during labor and childbirth (6). The burden of maternal and perinatal deaths is disproportionately higher in low- and middle-income countries (LMICs) compared to high-income countries (HICs). Therefore, improving the quality of care around the time of birth, especially in LMICs, has been identified as the most impactful strategy for reducing stillbirths, maternal and newborn deaths, compared with antenatal or postpartum care strategies (7).Monitoring Fetal Growth Research Paper
ORDER A PLAGIARISM-FREE PAPER HERE
Over the last two decades, women have been encouraged to give birth in health care facilities to ensure access to skilled health care professionals and timely referral should the need for additional care arise. However, accessing labor and childbirth care in health care facilities may not guarantee good quality care. Disrespectful and undignified care is prevalent in many facility settings globally, particularly for underprivileged populations, and this not only violates their human rights but is also a significant barrier to accessing intrapartum care services (8). In addition, the prevailing model of intrapartum care in many parts of the world, which enables the health care provider to control the birthing process, may expose apparently healthy pregnant women to unnecessary medical interventions that interfere with the physiological process of childbirth.
As highlighted in the World Health Organization (WHO) framework for improving quality of care for pregnant women during childbirth, experience of care is as important as clinical care provision in achieving the desired person-centered outcomes (9).
This up-to-date, comprehensive and consolidated guideline on intrapartum care for healthy pregnant women and their babies brings together new and existing WHO recommendations that, when delivered as a package of care, will ensure good quality and evidence-based care in all country settings. In addition to establishing essential clinical and non-clinical practices that support a positive childbirth experience, the guideline highlights unnecessary, non-evidence-based and potentially harmful intrapartum care practices that weaken women’s innate childbirth capabilities, waste resources and reduce equity.Monitoring Fetal Growth Research Paper
To ensure that each recommendation is correctly understood and applied in practice, the context of all context-specific recommendations is clearly stated within each recommendation, and the contributing experts provided additional remarks where needed.
In accordance with WHO guideline development standards, these recommendations will be reviewed and updated following the identification of new evidence, with major reviews and updates at least every five years.
At your prenatal ultrasound appointments, your sonographer is doing much more than counting fingers and toes -- she's taking lots of measurements of your baby to check on your child's growth, and make sure that everything's A-OK.
One of the most common measurements is crown-rump length, which is used in the first trimester, and measures your baby's size from head to tush. The reason it's important? "This measurement is extremely accurate in dating the pregnancy in the first trimester," says Michele Hakakha, M.D., an ob-gyn in Beverly Hills and author of Expecting 411. "It helps us determine if the size of the fetus matches up with the size it should be based on the patient's last menstrual period." If this number is considered off early on, that could indicate potential issues. "A smaller crown-rump length may signal an embryo that is not developing normally and may have a chromosomal problem, or it could mean that a woman's dates are off and she is not as far along as she thinks."
- Track your pregnancy, week by week!
After the first trimester, your baby will also have measurements taken of the diameter and circumference of her head, the circumference of her abdomen, and the length of her femur bone.
Those measurements will continue to be made as the pregnancy progresses, to make sure that your baby is growing along a predictable curve. "The computer within the ultrasound machine is capable of taking all the size measurements of the head, abdomen and femur, to give an estimate of size based on weeks of pregnancy," says Dr. Hakakha. "For example, if a woman who is 28 weeks pregnant goes in for an ultrasound, most of her baby's measurements should be equal to 28 weeks, as determined by the machine."Monitoring Fetal Growth Research Paper
As long as your baby's measurements are progressing along a normal growth curve, you have no reason to worry. "A cause for concern arises when measurements are either much larger or much smaller than anticipated," Dr. Hakakha says. "A smaller baby in the second and third trimesters, particularly a baby whose abdomen is measuring smaller, may not be getting everything he or she needs from its placenta. A larger baby, on the other hand, may signal the presence of diabetes or other conditions."
- Pregnancy books: Find them in our shop!
If your doctor thinks your measurements don't add up, she may request additional tests to determine if there's cause for concern -- for your health or your baby's. "Ultrasound is paramount in measuring the size and growth of babies because it helps practitioners become aware of other health conditions that may be hiding in a pregnant woman, allows us to initiate more testing, if necessary, and prepare for delivery," Dr. Hakakha says. These measurements will help ensure that you and your baby are healthy throughout the pregnancy and beyond.
Three recently completed longitudinal cohort studies have developed intrauterine fetal growth charts, one in the United States and two international. This expert review compares and contrasts the Eunice Kennedy Shriver National Institute of Child Health and Human Development Fetal Growth Studies, INTERGROWTH-21st and World Health Organization Multicentre Growth Reference Study conclusions in light of differences in aims, sampling frames, and analytical approaches. An area of controversy is whether a single growth reference is representative of growth, regardless of ethnic or country origin. The INTER GROWTH and World Health Organization Fetal studies used a similar approach as the World Health Organization Multicolored Growth Reference Study for infants and children, the aim of which was to create a single international reference for the best physiological growth for children aged 0-5 years. INTER GROWTH made the same assumption (ie, that there would be no differences internationally among countries or racial/ethnic groups in fetal growth when conditions were optimal). INTER GROWTH found differences in crown-rump length and head circumference among countries but interpreted the differences as not meaningful and presented a pooled standard. The World Health Organization Multicolored Growth Reference Study was designed to create a pooled reference, although they evaluated for and presented country differences, along with discussion of the implications. The Eunice Kennedy Shriver National Institute of Child Health and Human Development Study was designed to assess whether racial/ethnic-specific fetal growth standards were needed, in recognition of the fact that fetal size is commonly estimated from dimensions (head circumference, abdominal circumference, and femur length) in which there are known differences in children and adults of differing racial/ethnic groups. A pooled standard would be derived if no racial/ethnic differences were found. Highly statistically significant racial/ethnic differences in fetal growth were found resulting in the publication of racial/ethnic-specific derived standards. Despite all 3 studies including low-risk status women, the percentiles for fetal dimensions and estimated fetal weight varied among the studies. Specifically, at 39 weeks, the 50th percentile for estimated fetal weight was 3502 g for whites, 3330 g for Hispanics, 3263 g for Asians, and 3256 for blacks in the Eunice Kennedy Shriver National Institute of Child Health and Human Development Study, compared with 3186 g for INTER GROWTH and 3403 g for World Health Organization Multi centre Growth Reference Study. When applying these standards to a clinical population, it is important to be aware that different percentages of small- and large-for-gestational-age fetuses will be identified. Also, it may be necessary to use more restrictive cut points, such as the 2.5th or 97.5th, for small-for-gestational-age or large-for-gestational-age fetuses, respectively. Ideally, a comparison of diagnostic accuracy, or misclassification rates, of small-for-gestational-age and large-for-gestational-age fetuses in relation to morbidity and mortality using different criteria is necessary to make recommendations and remains an important data gap. Identification of the appropriate percentile cutoffs in relation to neonatal morbidity and mortality is needed in local populations, depending on which fetal growth chart is used. On a final point, assessment of fetal growth with a one-time measurement remains standard clinical practice, despite recognition that a single measurement can indicate only size. Ultimately, it is knowledge about fetal growth in addition to other factors and clinical judgment that should trigger intervention.Monitoring Fetal Growth Research Paper
Intrauterine growth restriction (IUGR) occurs in around 3 in every 100 pregnancies. Unborn babies with IUGR can grow so slowly in the womb that they are at risk of health problems. If the growth restriction is severe, the baby may have to be delivered, so it is also a cause of premature birth.
Causes of Intrauterine Growth Restriction
The majority of cases of IUGR are caused by failure of the placenta but there are also several other factors that could cause a baby's growth to be restricted:
- multiple pregnancy
- infection
- Antiphospholid Syndrome
- genetic problems or a congenital anomaly in the baby
- pre-existing medical problems in the mother such as high blood pressure, kidney disease, diabetes, heart disease, lung disease, chronic anaemia
- certain prescribed medications such as warfarin, some but not all anticonvulsants, and some anticancer drugs
- low pregnancy weight
- smoking or using drugs during pregnancy
- drinking alcohol during pregnancy.Monitoring Fetal Growth Research Paper
Around 10 in every 100 babies are small for gestational age. Most of these are small for normal reasons, such as the mother’s size and ethnicity, but around a third will be due to intrauterine growth restriction.
Signs and symptoms of Intrauterine Growth Restriction
IUGR is normally diagnosed during routine antenatal appointments. Your baby’s size is monitored throughout your pregnancy in your routine appointments. The midwife will palpate your stomach gently to feel the baby’s size, and they will measure the fundal height. The measure is then put on a chart that plots the growth. If there are any concerns the midwife will refer you for a scan. This does not necessarily mean something is wrong, but it is important to have the scan as more accurate way of assessing the baby's growth.
ORDER A PLAGIARISM-FREE PAPER HERE
Management of Intrauterine Growth Restriction
There is no 'treatment for IUGR. Instead you will have a management plan. If IUGR is suspected, you will have regular scans to look at the baby’s growth. The blood flow through the placenta will be checked with a uterine artery doppler test. If there is concern about growth then a plan will be implemented including regular scans, CTG monitoring and consultant appointments in antenatal clinic at the unit.
You will be told to closely monitor your baby’s movements.
If the growth restriction is severe, your healthcare team will recommend additional scans for monitoring of growth and baby well-being. They may recommend delivering the baby early.Monitoring Fetal Growth Research Paper
Fetal movements
It is very important to be aware of your baby’s pattern of movements and monitor this for change if you have been diagnosed with suspected IUGR.
A fetal ultrasound (sonogram) is an imaging technique that uses sound waves to produce images of a fetus in the uterus. Fetal ultrasound images can help your health care provider evaluate your baby's growth and development and monitor your pregnancy. In some cases, fetal ultrasound is used to evaluate possible problems or help confirm a diagnosis.
The first fetal ultrasound is usually done during the first trimester to confirm the pregnancy and estimate how long you've been pregnant. If your pregnancy remains uncomplicated, the next ultrasound is typically offered during the second trimester, when anatomic details are visible. If a problem is suspected, a follow-up ultrasound or additional imaging tests, such as an MRI, might be recommended.
There are two main types of fetal ultrasound exams:
- Trans vaginal ultrasound. With this type of fetal ultrasound, a wand like device called a transducer is placed in your vagina to send out sound waves and gather the reflections. Trans vaginal ultrasounds are used most often during early pregnancy. This type of ultrasound also might be done if a trans abdominal ultrasound didn't provide enough information.
- Trans abdominal ultrasound. A trans abdominal fetal ultrasound is done by moving a transducer over your abdomen.
Various other types of trans abdominal ultrasounds are available, including:Monitoring Fetal Growth Research Paper
- Specialized sonographic evaluation. This type of exam might be needed in specific circumstances, such as when a fetal abnormality is known or suspected. In this situation, a more detailed evaluation can provide additional information about the abnormality.
- 3D ultrasound. This exam provides a two-dimensional display of three-dimensional data. This type of ultrasound is sometimes used to help health care providers detect facial abnormalities or neural tube defects.
- Doppler ultrasound. A Doppler ultrasound measures slight changes in the ultrasound waves as they bounce off moving objects, such as blood cells. It can provide details about a baby's blood flow.
- Fetal electrocardiography. This exam provides a detailed picture of a baby's heart. It might be used to confirm or rule out a congenital heart defect.
Why it's done
First trimester ultrasound examination is done to evaluate the presence, size and location of the pregnancy, determine the number of fetuses, and estimate how long you've been pregnant (gestational age). Ultrasound can also be used for first trimester genetic screening, as well as screening for abnormalities of your uterus or cervix.
In the second or third trimester a standard ultrasound is done to evaluate several features of the pregnancy, including fetal anatomy. This exam is typically done between weeks 18 and 20 of pregnancy. However, the timing of this ultrasound might be altered for reasons such as obesity, which could limit visualization of the fetus.Monitoring Fetal Growth Research Paper
During the second and third trimesters, limited ultrasound evaluation might be needed when a specific question requires investigation. Examples include the evaluation of fetal growth and the estimation of amniotic fluid volume. A specialized or detailed exam is done when an anomaly is suspected based on your history or other prenatal exam results.
Your health care provider might use fetal ultrasound to:
- Confirm the pregnancy and its location. Some fetuses develop outside of the uterus, in the Fallopian tube. A fetal ultrasound can help your health care provider detect a pregnancy outside of the uterus (ectopic pregnancy).
- Determine your baby's gestational age. Knowing the baby's age can help your health care provider determine your due date and track various milestones throughout your pregnancy.Monitoring Fetal Growth Research Paper
- Confirm the number of babies. If your health care provider suspects a multiple pregnancy, an ultrasound might be done to confirm the number of babies.
- Evaluate your baby's growth. Your health care provider can use ultrasound to determine whether your baby is growing at a normal rate. Ultrasound can be used to monitor your baby's movement, breathing and heart rate.
- Study the placenta and amniotic fluid levels. The placenta provides your baby with vital nutrients and oxygen-rich blood. Too much or too little amniotic fluid — the fluid that surrounds the baby in the uterus during pregnancy — or complications with the placenta need special attention. An ultrasound can help evaluate the placenta and amniotic fluid around the baby.
- Identify birth defects. An ultrasound can help your health care provider screen for some birth defects.
- Investigate complications. If you're bleeding or having other complications, an ultrasound might help your health care provider determine the cause.
- Perform other prenatal tests. Your health care provider might use ultrasound to guide needle placement during certain prenatal tests, such as amniocentesis or chorionic villus sampling.
- Determine fetal position before delivery. Most babies are positioned headfirst by the end of the third trimester. That doesn't always happen, though. Ultrasound imaging can confirm the baby's presentation so that your health care provider can discuss options for delivery.Monitoring Fetal Growth Research Paper
Fetal ultrasound should be done only for valid medical reasons. Fetal ultrasound isn't recommended only to determine a baby's sex. Similarly, fetal ultrasound isn't recommended solely for the purpose of producing keepsake videos or pictures.
If your health care provider doesn't suggest a fetal ultrasound but you'd like the reassurance an ultrasound can provide, share your wishes with your care provider so that you can work together to determine what's best for you and your baby.
Risks
Diagnostic ultrasound has been used during pregnancy for many years and is generally considered safe when used appropriately. The lowest amount of ultrasound energy that provides an accurate assessment should be used.
Fetal ultrasound also has limitations. Fetal ultrasound might not detect all birth defects — or might incorrectly suggest a birth defect is present when it's not.Monitoring Fetal Growth Research Paper
How you prepare
You might be asked to drink a certain amount of fluid or avoid urinating before a fetal ultrasound, depending on the type of ultrasound. When scheduling your ultrasound, ask your health care provider for instructions.
Also be aware that fetal ultrasound can be done through the vagina (trans vaginal) or over the abdomen (trans abdominal), depending on why it's being done or the stage of your pregnancy. If you're having a trans abdominal ultrasound, consider wearing loose fitting clothing so that you can easily expose your abdomen.
What you can expect
During the procedure
During a transabdominal fetal ultrasound, you'll recline on an exam table and expose your abdomen. Your health care provider or technician will apply a special gel to your abdomen. This will improve the conduction of sound waves and eliminate air between your skin and the transducer.
Your health care provider or technician will move or scan the transducer back and forth over your abdomen. The sound waves reflected off your bones and other tissues will be converted into images on a monitor.Monitoring Fetal Growth Research Paper
Your health care provider or technician will measure your baby's anatomy. He or she might print or store certain images to document important structures. You'll likely be given copies of some of the images.
Depending on your baby's position and stage of development, you might be able to make out a face, hands and fingers, or arms and legs. Don't worry if you can't "see" your baby. Ultrasound images can be hard for an untrained observer to decipher. Ask your health care provider or technician to explain what's on the screen.
The procedure for other types of fetal ultrasound exams is similar. If you're having a trans vaginal ultrasound, however, you'll be asked to change into a hospital gown or undress from the waist down. You'll recline on an exam table and place your feet in stirrups. The transducer will be covered in a plastic sheath, like a condom, and be lubricated with gel. Your health care provider or technician will place the transducer in your vagina.Monitoring Fetal Growth Research Paper
Typically, a fetal ultrasound offers reassurance that a baby is growing and developing normally. If your health care provider wants more details about your baby's health, he or she might recommend additional tests.
Fetal monitoring
Your baby’s heart rate will be monitored throughout labour to make sure your baby is coping. Your midwife will watch for any marked change in the rate, which could be a sign that your baby is distressed and that something needs to be done.
It’s important to check your baby’s heartbeat during labour, as a change can be a sign the baby isn’t getting enough oxygen. This is called ‘fetal distress’.Monitoring Fetal Growth Research Paper
The heartbeat can be monitored a number of different ways:
Listening
The midwife does regular checks (every 15 to 30 minutes) by pressing an ear trumpet (often called a ‘Pinard horn’) or doppler (ultrasound) monitor to your abdomen to listen to your baby’s heartbeat.
This monitoring is recommended if your pregnancy has been healthy and normal and you are well.
Continuous external fetal monitoring
This is done by using an electronic monitor attached to a belt around your abdomen. This continuously records the baby’s heartbeat and your contractions on a paper printout. External monitoring is used if there are complications or there are risks of complications. Some monitors restrict your movements. If you are advised to have continuous monitoring, ask if there’s one available that lets you move around.Monitoring Fetal Growth Research Paper
Internal fetal monitoring
This uses an electronic monitor that attaches a probe through the vagina to the baby’s head. It should only be used if the external monitoring is problematic, the quality of the recording is poor, or in a twin pregnancy. It should not be used if you are HIV positive or hepatitis C positive.
Fetal scalp blood sampling
A few drops of blood are taken from your baby’s scalp (like a pin prick). This kind of monitoring gives an immediate report on the baby’s condition in labor. This test would be done if the doctors need more information than continuous monitoring provides. Sometimes this test needs to be repeated. The result will indicate if the baby needs to be born immediately.
Fetal growth restriction is a complex problem in modern obstetrics. It is a condition of sub optimal fetal growth based on a genetically predetermined potential and affects approximately 5% to 10% of pregnancies. It is traditionally defined as an estimated fetal weight less than the 10th percentile. Those pregnancies that are affected by growth restriction are associated with increased risk of perinatal morbidity and mortality. Because of this increased risk, these pregnancies are monitored more closely to try to identify those fetuses at the greatest risk of fetal demise and initiate delivery before this critical event. Although the ideal management strategy is still being determined, there are several modalities available to assist in assessment of the growth-restricted fetus. These include the non stress test test, biophysical profile, and Doppler velocimetry, most commonly of the fetal umbilical artery, in addition to sonographic growth assessment. The use of multiple fetal assessment tools may help improve the prediction of adverse outcomes and initiate delivery before cardiovascular collapse.Monitoring Fetal Growth Research Paper
You're pregnant. Congratulations! You'll undoubtedly spend the months ahead wondering how your baby is growing and developing. What does your baby look like? How big is he or she? When will you feel the first kick?
Fetal development typically follows a predictable course. Find out what happens during the first trimester by checking out this weekly calendar of events. Keep in mind that measurements are approximate.
Weeks 1 and 2: Getting ready
It might seem strange, but you're not actually pregnant the first week or two of the time allotted to your pregnancy. Yes, you read that correctly!Monitoring Fetal Growth Research Paper
Conception typically occurs about two weeks after your last period begins. To calculate your due date, your health care provider will count ahead 40 weeks from the start of your last period. This means your period is counted as part of your pregnancy — even though you weren't pregnant at the time.
Week 3: Fertilization
The sperm and egg unite in one of your Fallopian tubes to form a one-celled entity called a zygote. If more than one egg is released and fertilized or if the fertilized egg splits into two, you might have multiple zygotes.
The zygote typically has 46 chromosomes — 23 from the biological mother and 23 from the biological father. These chromosomes help determine your baby's sex and physical traits.
Soon after fertilization, the zygote travels down the Fallopian tube toward the uterus. At the same time, it will begin dividing to form a cluster of cells resembling a tiny raspberry — a morula.
Week 4: Implantation
The rapidly dividing ball of cells — now known as a blastocyst — has begun to burrow into the uterine lining (endometrium). This process is called implantation.Monitoring Fetal Growth Research Paper
ORDER A PLAGIARISM-FREE PAPER HERE
Within the blastocyst, the inner group of cells will become the embryo. The outer layer will give rise to part of the placenta, which will nourish your baby throughout the pregnancy.
Week 5: Hormone levels increase
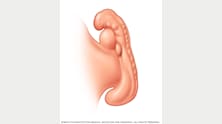
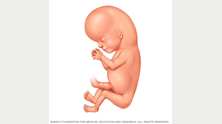
Fetal development three weeks after conception
The fifth week of pregnancy, or the third week after conception, the levels of HCG hormone produced by the blastocyst quickly increase. This signals your ovaries to stop releasing eggs and produce more estrogen and progesterone. Increased levels of these hormones stop your menstrual period, often the first sign of pregnancy, and fuel the growth of the placenta.
The embryo is now made of three layers. The top layer — the ectoderm — will give rise to your baby's outermost layer of skin, central and peripheral nervous systems, eyes, and inner ears.
Your baby's heart and a primitive circulatory system will form in the middle layer of cells — the mesoderm. This layer of cells will also serve as the foundation for your baby's bones, ligaments, kidneys and much of the reproductive system.
The inner layer of cells — the endoderm — is where your baby's lungs and intestines will develop.Monitoring Fetal Growth Research Paper
Week 6: The neural tube closes
Fetal development four weeks after conception
Growth is rapid this week. Just four weeks after conception, the neural tube along your baby's back is closing. The baby's brain and spinal cord will develop from the neural tube. The heart and other organs also are starting to form.
Structures necessary to the development of the eyes and ears develop. Small buds appear that will soon become arms. Your baby's body begins to take on a C-shaped curvature.
Week 7: Baby's head develops
Fetal development five weeks after conception
Seven weeks into your pregnancy, or five weeks after conception, your baby's brain and face are growing. Depressions that will give rise to nostrils become visible, and the beginnings of the retinas form.Monitoring Fetal Growth Research Paper
Lower limb buds that will become legs appear and the arm buds that sprouted last week now take on the shape of paddles.
Week 8: Baby's nose forms
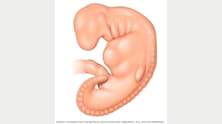
Fetal development six weeks after conception
Eight weeks into your pregnancy, or six weeks after conception, your baby's lower limb buds take on the shape of paddles. Fingers have begun to form. Small swellings outlining the future shell-shaped parts of your baby's ears develop and the eyes become obvious. The upper lip and nose have formed. The trunk and neck begin to straighten.
By the end of this week, your baby might be about 1/2 inch (11 to 14 millimeters) long from crown to rump — about half the diameter of a quarter.Monitoring Fetal Growth Research Paper
Week 9: Baby's toes appear
Fetal development seven weeks after conception
In the ninth week of pregnancy, or seven weeks after conception, your baby's arms grow and elbows appear. Toes are visible and eyelids form. Your baby's head is large but still has a poorly formed chin.
By the end of this week, your baby might be a little less than 3/4 inch (16 to 18 millimeters) long from crown to rump — the diameter of a penny.
Week 10: Baby's elbows bend
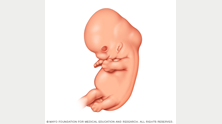
Fetal development eight weeks after conception
By the 10th week of pregnancy, or eight weeks after conception, your baby's head has become more round.
Your baby can now bend his or her elbows. Toes and fingers lose their webbing and become longer. The eyelids and external ears continue to develop. The umbilical cord is clearly visible.
Week 11: Baby's genitals develop
At the beginning of the 11th week of pregnancy, or the ninth week after conception, your baby's head still makes up about half of its length. However, your baby's body is about to catch up.Monitoring Fetal Growth Research Paper
Your baby is now officially described as a fetus. This week your baby's face is broad, the eyes widely separated, the eyelids fused and the ears low set. Buds for future teeth appear. Red blood cells are beginning to form in your baby's liver. By the end of this week, your baby's external genitalia will start developing into a penis or clitoris and labia majora.
By now your baby might measure about 2 inches (50 millimeters) long from crown to rump — the length of the short side of a credit card — and weigh almost 1/3 ounce (8 grams).
Week 12: Baby's fingernails form
Fetal development 10 weeks after conception
Twelve weeks into your pregnancy, or 10 weeks after conception, your baby is sprouting fingernails. Your baby's face now has taken on a more developed profile. His or her intestines are in the abdomen.
The perinatal literature includes several potentially confusing and controversial terms and concepts related to fetal size and growth. This article discusses fetal growth from an obstetric perspective and addresses various issues including the physiologic mechanisms that determine fetal growth trajectories, known risk factors for abnormal fetal growth, diagnostic and prognostic issues related to restricted and excessive growth and temporal trends in fetal growth. Also addressed are distinctions between fetal growth 'standard's and fetal growth 'references', and between fetal growth charts based on estimated fetal weight vs those based on birth weight. Other concepts discussed include the incidence of fetal growth restriction in pregnancy (does the frequency of fetal growth restriction increase or decrease with increasing gestation?), the obstetric implications of studies showing associations between fetal growth and adult chronic illnesses (such as coronary heart disease) and the need for customizing fetal growth standards.Monitoring Fetal Growth Research Paper
The environment in which a baby develops is not only important for its survival at birth but also for its long-term health. During pregnancy, it is important for the baby to receive the correct amount of nutrition and for it grow to an appropriate size. The baby communicates its changing nutritional needs and the mother’s body responds to this accordingly. This conversation between mother and baby is spoken in the language of hormones.
Why is fetal weight important during pregnancy?
Computer artwork showing a full-term fetus in the womb.
Several different hormones carefully regulate the growth of the fetus during pregnancy. Some hormones promote growth, while others have the opposite effect. It is vital the balance of these hormones is correct so that fetal growth occurs at a suitable pace throughout pregnancy. Hormones act to prevent fetal overgrowth and undergrowth by carefully controlling the supply of nutrients that pass across the placenta. The placenta acts as an interface between the mother and baby allowing regulated passage of oxygen and nutrients to the fetus. In addition, the placenta produces and responds to hormones that regulate fetal growth and development.
If a baby is born either too large (macrosomic) or too small (growth restricted), it can put you and your baby at greater risk of certain complications. Macrosomic babies often cause obstetric problems such as shoulder dystocia: a difficult labour in which significant medical intervention (possibly emergency Caesarean section) is needed for the baby’s shoulders and body to be delivered. Macrosomic babies have been shown to be more likely to develop later glucose intolerance (a condition often leading to diabetes mellitus) and obesity as adolescents and adults. Growth restricted babies are more at risk of health problems than normal sized babies and are also more prone to developing diseases such as hypertension, coronary heart disease and diabetes mellitus as adults.Monitoring Fetal Growth Research Paper
Insulin promotes fetal growth
Insulin, which is best known for regulating blood sugar levels, stimulates fetal growth and so a lack of this hormone can lead to a growth restricted baby. The primary sugar (glucose) that circulates in blood provides energy for a growing baby, which unlike its mother, is not able to make glucose for itself. The mother will have to supply all the glucose the baby needs for powering processes like tissue growth and laying down fat. During pregnancy, the mother’s body becomes less sensitive to the effects of insulin and so excess glucose is present in the maternal blood, available for passage across the placenta, but the fetus also produces insulin; so when glucose passes across the placenta, insulin stimulates its uptake into fetal tissues allowing it to be used as an energy source. This, in turn, allows tissue growth, or the glucose is converted and stored as fat. By keeping the fetal blood clear of glucose, fetal insulin stimulates the placenta to allow more glucose to pass to the fetus.
Some women can experience a type of diabetes that is specific to pregnancy, known as gestational diabetes. Insulin, like all hormones, works by attaching to receptors on target tissues in the body, much like a key fits a lock. In gestational diabetes, the receptors that insulin normally binds to do not work properly and glucose is not cleared out of the mother’s blood. This leaves excessive amounts of glucose in the mother’s blood, which passes across the placenta to the fetus; too much glucose can lead to a macrosomic baby. Overweight and obese women are more likely to suffer with gestational diabetes than normal weight women, but this problem can be managed by limiting weight gain during pregnancy with careful exercise and healthy eating habits. It is important to control this condition, but should it arise, medication (primarily metformin) can be used to treat it and reduce glucose levels.Monitoring Fetal Growth Research Paper
Insulin-like growth factors
The insulin-like growth factors are a family of hormones with a similar action to insulin, and like insulin, they also play a key role in fetal growth during pregnancy. Insulin-like growth factors are also known as ‘growth factors’ as they both stimulate the growth and survival of the fetus.
There are two types of insulin-like growth factor – IGF-I and IGF-II. Studies have shown that the higher the level of IGF-I in fetal blood, the greater the fetal weight at birth. Insufficient IGF-I during pregnancy results in a growth restricted baby, which struggles to grow after birth. However, cases of this are very rare and are usually a result of a genetic disorder. In normal pregnancy, IGF-I is thought to act as a ‘nutrient sensor’ checking which nutrients are present and how much of them are available, and then matching this to fetal demand. This is significant because the different types of nutrients the baby receives can be just as important as the overall amount. IGF-I is central to this effect because it can alter the passage of nutrients across the placenta, varying the amount and speed of transfer of the different types of nutrients, in response to changing fetal demand. The ability of IGF-I to change placental transport of nutrients can also be used to counteract the effects of under-nutrition; if the fetus is not getting enough nutrition to grow properly, IGF-I is able to sense this and increase the amount of nutrients passing across the placenta.
Unlike IGF-I, IGF-II levels do not seem to change in response to differences in nutrient availability or fetal nutrient demand nor is it correlated to fetal weight like IGF-I. This hormone helps the fetus grow by affecting the growth of the placenta. Because IGF-II stimulates the growth of the placenta, it allows more nutrients to pass to the fetus. If there is a lack of IGF-II, the placenta does not grow and develop correctly and so its function is compromised. This can result in a growth restricted baby that did not receive all the nutrition required during pregnancy. If too much IGF-II is present, it can lead to fetal overgrowth and a macrosomic baby; however, this is a rare occurrence and is only usually seen in genetic disorders, such as Beckwith-Wiedemann syndrome.Monitoring Fetal Growth Research Paper
The insulin-like growth factors work together to stimulate and control etal growth via changes in size and function of the placenta. IGF-II is important for placental growth and development, whereas IGF-I finely tunes what passes across the placenta. This means IGF-I levels respond to changes in both the maternal environment and fetal demand, ensuring the growing baby is supplied with everything it needs.
ORDER A PLAGIARISM-FREE PAPER HERE
Glucocorticoids
Other hormones, such as the steroid hormones corticosterone and cortisol, are important for fetal development during pregnancy. These steroids belong to a family of hormones, called the glucocorticoids, which are known to be associated with the regulation of stress. Unlike insulin and IGFs, glucocorticoids limit fetal growth and coordinate the development of fetal tissues and organs. As pregnancy nears term, a surge in glucocorticoids produced by the fetus can be detected. This naturally slows fetal growth, in favour of maturing and developing fetal tissues and organs. It is vital that the fetal tissues and organs go through this process at this time, in order for them to function properly outside of the womb. Women in Europe and the USA are given the glucocorticoid dexamethasone if labour begins before 37 weeks of pregnancy - this stimulates maturation of the baby’s tissues and organs (especially the lungs), so even if the baby arrives earlier than expected, the baby should be able to breathe and function outside of the womb. This medical intervention significantly decreases the mortality and morbidity rates of premature babies. Monitoring Fetal Growth Research Paper
Glucocorticoids switch the pattern of fetal development from tissue growth to specialisation; so instead of building the tissues, glucocorticoids help them mature, thus preparing the baby for life after birth. However, if the fetus is exposed to large amounts of glucocorticoids prematurely, the normal pattern of fetal growth is disturbed and fetal tissue development occurs incorrectly, which can have long-term health consequences. Stress triggers the production of cortisol from the mother’s adrenal glands and so high levels of cortisol cross the placenta and result in growth restricted babies and pre-term birth. This is why pregnant women should avoid stress wherever possible. Studies have also shown that in very stressful situations, such as natural disasters, pregnant women are more likely to have growth restricted babies that are born prematurely due to the large amounts of cortisol made by the mother. Babies that are born before term, especially if they have a low birth weight, are often less likely to survive after birth and may experience long-term health consequences, such as developmental problems and learning disabilities. Glucocorticoids are therefore vitally important to normal fetal growth and health; however, they must be present at the correct levels and at the correct time to ensure they do not have adverse effects on either the mother or the baby.
Prenatal Brain Development
Imagine that one day you decide to count nonstop until you get to one billion. Let's assume that you could count one number every second on average, so it would take you a billion seconds. After doing the math, this means that it would take approximately 32 years to count to one billion.
Now, let's consider the fact that one tiny cell in an embryo grows into a fully-developed brain with 100 billion cells by the time a baby is born. To put this into perspective, remember that it would take you roughly 32 years to count to one billion (averaging one number per second). This means it would take you about 3,200 years to count to 100 billion! Yet, in only nine months, a human brain - with 100 billion cells - is formed. This means that at least 250,000 brain cells are created every minute on average! Because of this rapid pace of development, proper prenatal care is essential to the development of an unborn child's brain.
The First Trimester
The first three months of pregnancy, or the first trimester, is when basic brain structure begins to form. In the first month, just 16 days after fertilization, an embryo forms the neural tube. The neural tube is the earliest nervous system tissue and eventually develops into the brain and the spinal cord.Monitoring Fetal Growth Research Paper
During the second month of development, the neural tube begins to differentiate into brain cells and nerve cells. The brain cells transform into recognizable brain structures - most notably, the cerebral cortex is formed. The cerebral cortex is the outer layer of the brain. By the third month, this basic brain development allows the embryo to display reflexes and react to its environment. At the end of the first trimester, hormones are released that will determine whether development will continue to occur as male or female.
The Second Trimester
The second trimester is the fourth, fifth, and sixth months of a pregnancy. During the course of the second trimester, the brain becomes fully developed. Even though the brain has not reached its full size, most of the neurons within the central nervous system are present. A neuron is another name for a nerve cell, or the cells that conduct electrical impulses and make up the brain, spinal column, and nerves.
During the fourth month, the fetus begins to prepare itself for the outside world. The fetus can experience sensory sensations such as sound, taste, and smells. By the fifth month, the fetus is learning to control its reactions to these sensory sensations and to control its movement. The ability to consciously react to sensory sensations becomes even stronger during the sixth month. During the sixth month, another major mark of brain development occurs; the cerebral cortex splits into two separate hemispheres. Some researchers believe that the fetus develops the ability to remember at this stage.Monitoring Fetal Growth Research Paper
While you might think of child development as something that begins during infancy, the prenatal period is also considered an important part of the developmental process. Prenatal development is a time of remarkable change that helps set the stage for future psychological development. The brain develops over the course of the prenatal period, but it will continue to go through more changes during the early years of childhood
Let's take a closer look at the major stages and events that take place during the prenatal period of development. The process of prenatal development occurs in three main stages.
The first two weeks after conception are known as the germinal stage, the third through the eighth week is known as the embryonic period, and the time from the ninth week until birth is known as the fetal period.
Germinal Stage
The germinal stage begins at conception when the sperm and egg cell unite in one of the two Fallopian tubes. The fertilized egg, known as a zygote, then moves toward the uterus, a journey that can take up to a week to complete. Cell division begins approximately 24 to 36 hours after conception.
Within just a few hours after conception, the single-celled zygote begins making a journey down the Fallopian tube to the uterus where it will begin the process of cell division and growth. Through the process of mitosis, the zygote first divides into two cells, then into four, eight, sixteen, and so on. A significant number of zygotes never progress past this early part of cell division, with as many as half of all zygote's surviving less than two weeks.Monitoring Fetal Growth Research Paper
Once the eight-cell point has been reached, the cells begin to differentiate and take on certain characteristics that will determine the type of cells they will eventually become.
As the cells multiply, they will also separate into two distinctive masses: the outer cells will eventually become the placenta while the inner cells will form the embryo.
Cell division continues at a rapid rate and the cells then develop into what is known as a blastocyst. The blastocyst is made up of three layers:
- The ectoderm (which will become the skin and nervous system)
- The endoderm (which will become the digestive and respiratory systems)
- The mesoderm (which will become the muscle and skeletal systems).
Finally, the blastocyst arrives at the uterus and attached to the uterine wall, a process known as implantation.
Implantation occurs when the cells nestle into the uterine lining and rupture tiny blood vessels. The connective web of blood vessels and membranes that form between them will provide nourishment for the developing being for the next nine months. Implantation is not always an automatic and sure-fire process.Monitoring Fetal Growth Research Paper
Researchers estimate that approximately 60 percent of all natural conceptions never become properly implanted in the uterus, which results in the new life ending before the mother is ever aware she is pregnant.
When implantation is successful, hormonal changes halt a woman’s normal menstrual cycle and cause a whole host of physical changes. For some women, activities they previously enjoyed such as smoking and drinking alcohol or coffee may become less palatable, possibly part of nature’s way of protecting the growing life inside her.
Embryonic Stage
At this point, the mass of cells is now known as an embryo. The beginning of the third week after conception marks the start of the embryonic period, a time when the mass of cells becomes distinct as a human. The embryonic stage plays an important role in the development of the brain.
The embryo begins to divide into three layers each of which will become an important body system. Approximately 22 days after conception, the neural tube forms. This tube will later develop into the central nervous system including the spinal cord and brain.Monitoring Fetal Growth Research Paper
The neural tube begins to form along an area known as the neural plate. The earliest signs of development of the neural tube are the emergence of two ridges that form along each side of the neural place. Over the next few days, more ridges form and fold inward until a hollow tube is formed. Once this tube is fully formed, the cells begin to form near the center. The tube begins to close and brain vesicles form. These vesicles will eventually develop into parts of the brain including the structures of the fore brain, mid brain, and hind brain.
Around the fourth week, the head begins to form quickly followed by the eyes, nose, ears, and mouth. The cardiovascular system is where the earliest activity begins as the blood vessel that will become the heart start to pulse.
During the fifth week, buds that will form the arms and legs appear.
By the time the eighth week of development has been reached, the embryo has all of the basic organs and parts except those of the sex organs. It even has knees and elbows! At this point, the embryo weighs just one gram and is about one inch in length.Monitoring Fetal Growth Research Paper
By the end of the embryonic period, the basic structures of the brain and central nervous system have been established. At this point in development, the basic structure of the central and peripheral nervous system are also defined.
Research has shown that the production of neurons begins around day 42 after conception and is mostly complete sometime around the middle of pregnancy.
As neurons form, they migrate to different areas of the brain. Once they have reached the correct location, they begin to form connections with other neural cells, establishing rudimentary neural networks.
Fetal Stage
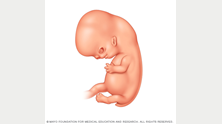
Once cell differentiation is mostly complete, the embryo enters the next stage and becomes known as a fetus. The fetal period of prenatal develop marks more important changes in the brain. This period of development begins during the ninth week and lasts until birth.
The early body systems and structures established in the embryonic stage continue to develop. It is at this point in prenatal development that the neural tube develops into the brain and spinal cord and neurons continue to form. Once these neurons have formed, they begin to migrate to their correct locations. Synapses, or the connections between neurons, also begin to develop.Monitoring Fetal Growth Research Paper
It is during the period between the 9th and 12th week at the earliest reflexes begin to emerge and the fetus begins to make reflexive motions with his arms and legs.
This stage of prenatal development lasts the longest and is marked by amazing change and growth. During the third month of gestation, the sex organs begin to differentiate and by the end of the month, all parts of the body will be formed. At this point, the fetus weight around three ounces. The fetus continues to grow in both weight and length, although the majority of the physical growth occurs in the later stages of pregnancy.
The end of the third month also marks the end of the first trimester of pregnancy. During the second trimester or months four through six, the heartbeat grows stronger and other body systems become further developed. Fingernails, hair, eyelashes, and toenails form. Perhaps most noticeably, the fetus increases quite dramatically in size, increasing about six times in size.
So what's going on inside the brain during this important period of prenatal development? The brain and central nervous system also become more responsive during the second trimester. Around 28 weeks, the brain starts to mature faster with an activity that greatly resembles that of a sleeping newborn.
During the period from seven months until birth, the fetus continues to develop, put on weight, and prepare for life outside the womb. The lungs begin to expand and contract, preparing the muscles for breathing.
A Word From Very well
The prenatal period of development is a time of physical growth, but what's going on inside the brain is critical for future psychological development. The brain development that takes place during the prenatal period helps set the course for what will take place outside the womb.Monitoring Fetal Growth Research Paper
While prenatal development usually follows this normal pattern, there are times when problems or deviations occur. Learn more about some of the problems with prenatal development. Disease, malnutrition, and other prenatal influences can have a powerful impact on how the brain develops during this critical period.
But brain development does not end at birth. There is a considerable amount of brain development that takes place postnatally including growing in size and volume while changing in structure. The brain grows by about four times the size between birth and preschool. As children learn and have new experiences, some networks in the brain are strengthened while other connections are pruned.Monitoring Fetal Growth Research Paper